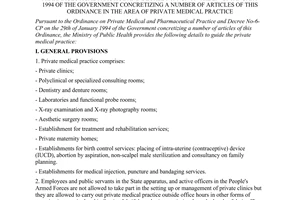
Nội dung toàn văn Circular No. 15/1999/TT-BYT of July 31, 1999, guiding the implementation of the ordinance on private practice of medicine and pharmacy and The Governments Decree No. 06/CP of January 29, 1994 detailing a number of articles of the ordinance on private practice of medicine and pharmacy with respect to the practice of medicine
|
THE
MINISTRY OF PUBLIC HEALTH |
SOCIALIST
REPUBLIC OF VIET NAM |
|
No: 15/1999/TT-BYT |
Hanoi, July 31, 1999 |
CIRCULAR
GUIDING THE IMPLEMENTATION OF THE ORDINANCE ON PRIVATE PRACTICE OF MEDICINE AND PHARMACY AND THE GOVERNMENT’S DECREE NO. 06/CP OF JANUARY 29, 1994 DETAILING A NUMBER OF ARTICLES OF THE ORDINANCE ON PRIVATE PRACTICE OF MEDICINE AND PHARMACY WITH RESPECT TO THE PRACTICE OF MEDICINE
Pursuant to the September 30, 1993 Ordinance
on private practice of medicine and pharmacy;
Pursuant to the Government’s Decree No. 06/CP of January 29, 1994 detailing a
number of Articles of the Ordinance on private practice of medicine and
pharmacy;
The Ministry of Health hereby guides the private practice of medicine as
follows:
Chapter I
THE GENERAL PROVISIONS
Article 1.- Forms of private medical establishments:
1. The private hospitals
- General hospitals.
- Specialized hospitals.
2. The general consultation clinic means a medical examination clinic with various specialized fields.
3. The specialized medical consultation clinic:
- The internal disease examination clinic, including:
+ The general internal disease examination room.
+ Rooms for examination of internal organs.
+ The family medical consultation room.
+ The via-telephone medical consultancy room.
- The surgical examination room.
- The obstetric examination and family planning room.
- The teeth-jaw- face examination room.
- The eye examination room.
- The ear-nose-throat examination room.
- The plastic surgery examination room.
- The convalescence and functional rehabilitation examination room.
- The image diagnosis-examination room.
- The bio-chemical, hematological, micro-organism and microtamic laboratory.
4. The maternity homes
5. Medical services
- The false teeth-making room
- The injection and bandage replacement
- Healthcare services provided at families.
Article 2.- Enterprises investing in the construction of private medical examination and treatment establishments and private medical practitioners are encouraged to do so and entitled to preferential treatment under the Domestic Investment Promotion Law of May 20, 1998. The heads of private medical examination and treatment establishments must be fully qualified for the occupational practice suited to each forms specified in this Circular.
Article 3.- State officials and on-active-service officers of the People’s Armed Forces are not allowed to participate in the establishment or management of private hospitals and/or medical examination and treatment establishments set up under the Private Enterprises Law and the Companies Law (or under the Law on Enterprises when it comes into force), but they may sign contracts with private hospitals and/or medical examination and treatment establishments to work thereat outside the official working hours or may register to practice their jobs outside the official working hours in other forms of organizations if they are so permitted in writing by their bosses.
Article 4.- The medical examination and treatment establishments must have signboards as prescribed, must publicize and keep to the hospital fee levels as well as the scope of prescribed professional practices. The hospital fee levels and scope of professional practices must be approved by the authorities competent to issue the "certificates of eligibility and qualifications for setting up private medical establishments."
Article 5.- The private medical examination and treatment establishments shall be allowed to start their operation only after being granted the certificates of eligibility and qualifications for setting up private medical establishments by the competent medical authorities.
Article 6.- All private medical establishments shall have to make registration and pay fees for the evaluation of eligibility and qualifications for being granted licenses to set up private medical practice establishments as jointly stipulated by the Ministry of Finance and the Ministry of Health.
Chapter II
CRITERIA, CONDITIONS AND SCOPE OF PROFESSIONAL PRACTICE OF PRIVATE MEDICAL ESTABLISHMENTS
Article 7.- Hospitals: Hospitals are establishments which provide medical examination and treatment for in-patients and out-patients as well. A hospital may be a general hospital or a specialized hospital.
1. Criteria:
The hospital director must be a general or specialized physician who has practiced at hospitals for 5 years.
The department head must be a specialized physician who has practiced at lawful medical examination and treatment establishment(s) for 5 years, including 3 years for the practice of his/her speciality.
2. Conditions:
- A hospital shall have at least 21 beds.
- The organization and personnel should be suitable to the hospital size.
- The infrastructure and medical equipment shall comply with the provisions in the Hospital Regulations issued together with Decision No. 1895/1997-BYT-QD of September 19, 1997.
A hospital must have all the following:
+ The medical examination- emergency department.
+ Therapy departments.
+ The pre-clinical departments.
+ Power and water supply systems, fire-fighting facilities and devices, waste treatment system.
+ Medical equipment for each department (at least equal to the district-level medical network) as prescribed by the "Regulation on lists of medical equipment for the provincial and district general hospitals, the regional general examination rooms, commune health stations", issued together with Decision No. 1419/BYT-QD of August 23, 1996 of the Health Minister.
3. Scope of professional practice:
Shall comply with the list of professional operations permitted by the Ministry of Health. Hospitals must admit patients in emergency cases and may transfer them to other hospitals only after giving them the first-aid and emergency care.
Article 8.- The general consultation clinic means a medical examination and treatment establishment which has many (at least 2) specialized consultation rooms, and is managed by a director.
1. Criteria:
The general consultation clinic director must be a general or specialized physician who has practiced at hospital(s) for 5 years; the specialized consultation clinic head must be a specialized physician who has practiced at lawful medical examination and treatment establishment(s) for 5 years, including 3 years for practice of his/her specialty.
2. Conditions:
Infrastructure: The establishment must have enough land area. Its equipment must be up to the standards and conditions of those for the specialized consultation clinic. In addition to specialized consultation rooms, a general consultation clinic must have the waiting room, emergency room, a confinement room (with not more than 10 beds and the confinement for not more than 24 hours), adequate WCs, power and water supply systems, waste treatment facility in order to ensure the environmental hygiene.
3. Scope of professional practice:
Practicing jobs according to the list of specialties already approved.
Article 9.- The internal disease examination clinic:
The internal disease examination clinic includes the following types:
- The general internal disease consultation room.
- Rooms for examination of internal organs.
- The family medical consultation room.
- The via-telephone medical consultancy room.
1. Criteria:
The medical practice registrants must be general or specialized physicians who have practiced at lawful medical examination and treatments for 5 years.
In high-mountain areas, those assistant-physicians who have practiced at medical examination and treatment establishments for 5 years or physicians who have practiced for 3 years may register for their professional practice. The assistant-physicians must not practice the via-telephone medical consultancy.
2. Conditions:
a/ The general internal disease consultation room and rooms for examination of internal organs must be equipped with minimum professional instruments and the first-aid and anti-shock medicine boxes. Each must have at least 1 separate examination room of 10m2, equipped with the examination bed and a desk. It must be airy, tidy, well lighted, constructed with WC(s) and separately from the family residence area.
b/ The family consultation room must be equipped with minimum professional instruments as well as first-aid and anti-shock medicine boxes.
3. Scope of professional practice:
a/ The general internal disease examination room and the family medical consultation room:
- Health and family planning consultancy.
- Health management.
- Providing first-aids, emergency, examination and making prescriptions, treatment of common diseases, not to practice specialized operations. Upon detection of cases which go beyond its capacity, transferring such patients to specialized clinics or higher-level medical establishments.
- Surgical examination: Providing first-aid to cases of bone fractures, without starch setting and without any minor operations.
- Providing obstetrical examination: fetus check-ups, obstetric management, not providing deliveries.
- Tooth examination, not performing tooth extraction.
- Ear-nose-throat examination; endoscopy; not lancing or slitting inflammation in middle ears.
- Making simple tests with testing papers.
- Taking illness samples and sending them for testing, without puncturing for samples.
- Electrocardiography, microwave diagnosis, etc. Separate certiticates are not required, but the certificates of professional fostering and practice issued by lawful medical examination and treatment establishments are required and such specialties have been permitted for inclusion into the scope of professional practice by the certificate-granting agencies.
b/ Rooms for examination of internal organs: To provide examination, diagnosis and treatment of illnesses under the approved specialties.
c/ The via-telephone medical consultancy room: Physicians only provide consultancy on specialties which have been registered and which they have been trained in.
Article 10.- Surgical examination rooms
1. Criteria:
The practitioners must be surgeons who have practiced their jobs at lawful medical examination and treatment establishments for 5 years, including 3 years for practice of surgery.
2. Conditions:
Besides the conditions on facilities and equipment as well as material foundations prescribed in Article 9 of this Circular, a surgical examination room must be equipped with minor-operation tools and room, the emergency and confinement rooms, with particular attention paid to the sterilizing techniques.
3. Scope of professional practice:
- Providing surgical first-aid and emergency treatment.
- Checking and treating common wounds.
- Starch-setting for minor bone fractures.
- Starch removing at the instruction of starch-setters.
- Thread-cutting small hemorrhoids; operating on cysts.
- Not lancing big diffuse abscesses or sores.
Article 11.- Obstetric examination rooms- Family planning rooms:
1. Criteria:
Those who register for such professional practice must be physicians who have practiced the jobs at lawful medical examination and treatment establishments for 5 years, including at least 3 years for obstetric practice.
In high-mountain regions, assistant-obstetricians or intermediate-level midwives who have practiced obstetrics for 5 years may register for the practice of such jobs.
2. Conditions:
To be equipped with examination couchs, instruments and perform minor-obstetric minor-operations. Apart from the consulting room, there is also the room for performance of minor operations. Apart from the common first-aid medicines, there must be medicines for obstetric emergencies.
3. Scope of professional practice:
- Consultancy on health education and family planning.
- Obstetric emergencies treatment.
- Fetus examination, obstetric management.
- Examination and treatment of common gynaecological diseases.
- Vagina medicament placing.
- Cauterization of uterine cavity.
- Uterine cavity endoscopy.
- IUD placing.
- Under 15 day-embryo siphonage.
- Non-knife vasectomy.
- No abortion, non-embryocide, not removing IUDs, not performing female sterilization.
- Not performing child deliveries at consulting rooms.
Article 12.- Tooth-jaw-face examination rooms:
1. Criteria:
Those who register for such professional practice must be tooth-jaw-face physicians, who have practiced their jobs at lawful establishments for 5 years.
In high-mountain regions, assistant teeth-jaw-face doctors who have practiced the jobs for 5 years or specialized physicians who have practiced such jobs for 3 years may register to practice such jobs.
2. Conditions:
- To be fully equipped with instruments and equipment for dentistry and denture making (if false teeth are made).
- To be equipped with minor-operation room and working room suitable to the scope of professional practice.
3. Scope of professional practice:
- Examination and treatment of common diseases, providing first-aid and emergency treatment of jaw and face wounds.
- Performing minor operations, erasing small wound scars.
- Re-setting jaw joints.
- Facial laser therapy.
- Treatment of tooth and gum diseases.
- Lancing/slitting abscesses, tooth scaling, tooth extraction.
- Making false teeth, dentures.
Article 13.- Ear-nose-throat examination rooms:
1. Criteria:
Those who register to practice the jobs must be ear-nose-throat physicians who have practiced at hospitals for 5 years, including at least 3 years for practice of such jobs.
2. Conditions:
To be fully equipped with instruments and tools for specialized examinations and operations, with the minor-operation room.
3. Scope of professional practice:
- Emergency treatment of ear, nose and throat diseases.
- Examination and treatment of common diseases.
+ Sinusitis, sinus pricking, pricking and siphonating substances from benign tumors.
+ Lancing/slitting inflations in middle ears.
+ Lancing/slitting amygdale abscesses.
+ Cutting simple polypuses, atherosclerosis, cyst, fat excrescene in the ear, nose or throat area.
+ Epistaxis coagulation.
+ Removing extraneous objects from ear, nose, throat areas not removing extraneous objects from larynx, cesophagus.
+ Heat or laser therapy of throat diseases.
+ Suturing neck wounds of under 5cm.
+ Adenoidectomy.
Article 14.- The specialized eye examination rooms:
1. Criteria:
The practitioners must be ophthalmologists who have practiced at hospitals for 5 years, including 3 years for opthalmological practice.
In high-mountain regions, the assistant-ophthalmologists who have had 5 years for opthalmological practice may practice the job.
2. Conditions
- To be fully equipped with instruments and tools for eye examination and treatment.
- To be provided with enough medicines for ophthalmological emergency, treatment.
- To be equipped with minor-operation room.
3. Scope of professional practice:
- Providing emergency and ordinary treatment of eye diseases.
- Giving injections under cornea, close to eyeball, behind eyeball.
- Removing extraneous objects in cornea, lancing styes, entropion surgery.
- Cleaning tear glands.
Article 15.- The specialized plastic and aesthetic surgery rooms mean establishments where beauty services shall be provided by physicians
Beauty services on face skin care, bridal make-ups, etc. are not subject to the eligibility certificates granted by the medical service. Such establishments are not allowed to perform lip puncture, eyelid puncture, black-reads removing, other services which cause bleeding.
1. Criteria:
The practitioners must be physicians who have practiced their jobs at hospitals for 5 years, including 3 years for practicing the plastic surgery or aesthetic surgery.
2. Conditions:
- To be equipped with facilities and equipment suited to the professional practice.
- The establishment must be sterile, furnished with operation room(s), confinement room, waiting room.
3. Scope of professional practice:
- Lip puncture, eyelid puncture, black-reads removing, beauty services which cause bleeding.
- Hair transplanting.
- Raising cheek bones, nose bridges
- Face skin stretching through operation.
- Treating wrinkles on upper and/or lower eye lids, making one-lid eyes into two-lid eyes.
Article 16.- Specialized convalescence and functional rehabilitation clinics.
1. Criteria:
The practitioners must be physicians specialized in functional rehabilitation, who have practiced their jobs at lawful medical establishments for 5 years, including at least 3 years for practicing convalescence and functional rehabilitation.
2. Conditions:
In addition to the requirements prescribed at Point a, Clause 2, Article 9 of this Circular, the convalescence and functional rehabilitation clinic must be fully furnished with rooms and instruments as well as facilities suited to the scope of professional practice.
3. Scope of professional practice
- Tending central and functional nerse syndromes.
- Tending chronic mascular-bone-joint diseases.
- Post- surgery care requiring further functional rehabilitation.
- Performing medical techniques:
+ Massage, digital puncture, acupuncture.
+ Approved physio-therapy methods.
+ Therapy operations.
Article 17.- The image diagnosis room: The image diagnosis room is the establishment where diseases are diagnosed and therapy results are monitored by X-ray, micro-wave radioscopic, endoscopie… equipment.
1. Criteria:
Those who register to practice image diagnosis must be physicians specialized in X-ray and have practiced their jobs for 5 years.
In high-mountain regions, physicians who have practiced their jobs at lawful medical examination and treatment establishments for 5 years, including at least 3 years for practice of X-ray, may register to practice image diagnosis.
2. Conditions:
- To be fully equipped with personal protection devices, the X-ray room up to the radiation safety standards, and equipment reaching the standards of at least district level.
- The infrastructure must be absolutely safe: There must be the waiting room, the X-ray room, the film developing and photo printing room, the film reading room, etc. The equipment room must be at least 3.5m high, have its wall pasted with barite, have the lead door and high and airy floor.
3. Scope of professional practice:
- X-ray diagnosis, topographic examination...
- Doppler microwave diagnosis.
- Non-use of vena optical reflection.
- Non-puncture guided by microwaves, non-performance of endoscopic operations, non-brouchoscopy, non-X intervention which cause bleeding.
Article 18.- The laboratories: The laboratories are establishments assisting the diagnosis and monitoring therapy, covering hematology, biochemistry, micro organism, morbid anatomy.
1. Criteria:
Those who register for lab practice must be physicians or pharmacists, bachelor of biology or bio-chemistry, who have practiced laboratory tests for 5 years at lawful medical examination and treatment establishments.
In the high-mountain regions, the practitioners must be physicians, pharmacists, bachelor of biology or bio-chemistry, who have practiced at lawful medical examination and treatment establishments for 5 years, including 2 years for specialty practice.
2. Conditions:
- To be equipped with minimum medical equipment (equivalent to the district-level laboratory).
- The infrastructure must be up to the standards of a lab. Its design, architecture and organization must ensure the labor safety as prescribed for scientific experiments. Apart from the laboratory area, attention should be paid to such support areas as power and water supply, fire prevention and fight systems.
3. Scope of professional practice:
Performing blood, bio-chemical, micro-biological and parasitic tests, morbid anatomy.
Article 19.- The maternity homes.
Maternity homes are places for child delivery and obstetric management and care.
1. Criteria:
The practitioners must be obstetricians, intermediate-level midwives who have practiced their jobs at obstetric establishments for 5 years.
In high-mountain regions, the obstetricians and intermediate-level midwives who have practiced their jobs at obstetric establishments for 3 years may register to run private maternity homes.
Persons who register to set up maternity homes must be full-time practitioners (not persons who are allowed to register only to practice their jobs outside the official working hours).
2. Conditions:
- Infrastructure: There must be rooms for waiting, delivery and post-natal cares which must be hygienic, sterile and airy.
- Facility and equipment: There must be delivery tables, delivery kits, instruments for fetus examination and minor-operations, medicine boxes for general emergencies and obstetric emergencies.
3. Scope of professional practice
- Fetus examination, obstetric management.
- Obstetric emergency and first-aid treatment.
- Giving anti-tetanus injection.
- Making proteine test.
- Performing ordinary delivery.
- Post-natal and post-miscarriage placenta remainer scooping.
- Not allowed to perform abortion.
- If obstetricians are available, difficult childbirths, under-15-day embryo siphonage.
IUD placing may be performed; not allowed to remove IUD and perform type-I obstetric operation.
Article 20.- Medical services: The medical services mentioned in this Circular are those provided at doctors’ prescription.
1. Criteria:
Those who register to set up establishments to provide services on injections, bandage changes must be nurses who have practiced their jobs at lawful medical examination and treatment establishments for 2 years.
Those who register to set up denture rooms must be dental technicians who have practiced their jobs before 1980, with the written certification by the local administration.
Those who register to provide healthcare services at home must possess professional degrees suitable to the services applied for.
2. Conditions:
- Injection and bandage change establishments:
+ There must be a room of at least 8m2.
+ Be fully equipped with instruments and ensuring sterilization.
+ Having emergency medicine boxes, room for treating injection shocks.
- The denture rooms: The establishments must satisfy the size requirements, having the separate denture room or workshop equipped with denture instruments.
3. Scope of professional practice:
- Injection, bandage change services; only provided at doctors’ prescription, not allowed to give medical examinations and prescriptions.
- Denture service: only allowed to make false teeth, not to examine and treat dental diseases or to perform tooth extraction.
- Providing healthcare services at home: at doctors’ prescriptions.
Chapter III
COMPETENCE TO GRANT CERTIFICATES OF ELIGIBILITY AND QUALIFICATIONS FOR SETTING UP PRIVATE MEDICAL ESTABLISHMENTS
Article 21.- The competence to grant certificates of eligibility and qualifications for setting up private medical establishments (called "the eligibility and qualification certificate " for short):
1. The Minister of Health shall grant "the eligibility and qualification certificates" to private hospitals and medical examination and treatment establishments set up under the Law on Private Enterprises and the Law on Companies (or under the Law on Enterprises when it takes effect).
2. The directors of the Health Services of the provinces and centrally-run cities (referred collectively to as the provincial level) shall grant the eligibility and qualification certificates to all other forms, except those mentioned in Clause 1, this Article.
3. The Ministry of Health shall set up the Advisory Council to assist the Minister in considering the criteria and conditions for granting the certificates. The Council is composed of a vice minister as its chairman, the director of the Department of Therapy as its permanent vice-chairman, a representative of the Executive Committee of the Vietnam Medicine and Pharmacy Society and others as its members.
4. The provincial-level Health Services shall set up Advisory Councils to assist the Service directors in considering the criteria and conditions for granting the certificates. Such a council is composed of a member of the leadership of the Service as its chairman, the head of the Medical Operation Section or the head of the Section for Management of the Private Medical or Pharmaceutical Establishments as its vice-chairman, a representative of the provincial Medicine and Pharmacy Society and others as its members.
Article 22.- The dossiers of application for the "professional practice eligibility and qualification certificate" shall be decided by the Minister of Health:
1. The application for setting up a hospital.
2. The application for evaluation and consideration for being granted the "professional practice eligibility and qualification certificate".
3. The hospital’s charter
4. The economic and technical feasibility study report: It must contain the following contents:
- The necessity to make investment.
- The objectives of the project.
- The signboard, location, form of investment, plan on infrastructure construction.
- The functional areas and sections, the number of hospital beds.
- Support constructions (electricity and water supply, fire prevention and fighting, waste treatment, paths, scapes.
- The construction costs.
- The implementation tempo.
- The granted certificate of waste treatment, radiation safety, fire prevention and fighting.
- Medical equipment.
- Appellations of equipment, the quantity, prices thereof, the total value of investment in equipment.
- The managerial apparatus, the personnel and organization section.
- The investment capital and financial analysis.
- The social and economic efficiency.
5. The detailed scope of professional practice.
6. The list of the Managing Board and the directorate (with CVs).
7. (Notarized) copies of diplomas, professional certificates, practice duration and health certificates of director, department heads, physicians, pharmacists and other officials of university degree, contracts and other relevant certificates.
8. Recommendation paper of the Medicine and Pharmacy Society.
Article 23.- The procedures for evaluation before granting the "professional practice eligibility and qualification certificates" to medical examination and treatment establishments, signed by the Minister of Health:
1. After completing all work on infrastructure construction, equipment, organization and personnel, the directors of private medical establishments (according to provisions in Clause 1, Article 21) shall submit their full dossiers to the provincial-level Health Services. The directors of the provincial Health Services shall set up the evaluation team composed of necessary members (including a representative of the Medicine and Pharmacy Society) to conduct direct evaluation at the applying establishments.
2. The evaluation contents:
a/ The legal bases.
b/ The dossiers of application for establishment (as prescribed in Article 22).
c/ Infrastructure and environmental hygiene conditions.
d/ Organization- personnel.
e/ Medical equipment and instruments.
f/ Detailed scope of professional practice.
3. The evaluation report shall include the following major details:
a/ Time and revenue.
b/ Composition:
- The evaluation team.
- Representative of the evaluated agency.
c/ The results of evaluation of the six contents (inscribed in details).
d/ Conclusions and proposals.
4. Upon the completion of the evaluation, the provincial-level Health Services shall send the recommendation papers enclosed with the evaluation reports and the complete dossiers of the evaluated establishments to the Ministry of Health.
All documents must be sent in their originals or notarized copies.
Article 24.-
1. The dossiers of application for the "professional practice eligibility and qualification certificates" decided by provincial-level Health service directors for various forms of private medical establishments shall include:
a/ The application for professional practice, clearly stating the location and scope of professional practice.
b/ The (notarized) copies of diplomas, specialty certificates.
c/ CVs and health certificates.
d/ The permits for professional practice outside the official working hours if the applicants are State officials or employees.
e/ The written exposition: location, establishment, equipment, organization and personnel, and scope of professional practice.
This can be stated in the application if the establishment shall perform simple professional practice.
f/ The recommendation paper of the Medicine and Pharmacy Society.
2. The procedures for evaluation to be granted the professional practice certificates signed by the provincial Health Service directors:
a/ The medical practice establishments shall file their dossiers to the provincial-level Health Services which shall set up evaluation teams and conduct the direct evaluation at the applying establishments.
b/ The evaluation contents and report shall comply with Clauses 2 and 3 of Article 23.
Article 25.- Validity duration of the professional practice eligibility and qualification certificates:
1. A professional practice eligibility and qualification certificate granted by the Minister of Health shall be valid for 5 years.
A professional practice eligibility and qualification certificate granted by a provincial-level Health Service director shall be valid for 3 years.
2. Three months before the expiry of their certificates, the establishments shall have to carry out procedures for consideration of the re-granting of their certificates.
Article 26.- The professional practice certificates shall be addressed and kept as follows:
- The professional practice certificate signed by the Minister of Health shall be made in 4 copies: 1 copy is addressed to the provincial People’s Committee, 1 to the provincial-level Health Service, 1 to the involved person and 1 kept at the Department of Therapy.
- The certificate of other forms shall be made in 3 copies: 1 is kept at the provincial-level Health Service, 1 is addressed to the involved person, 1 to the district Health Service.
Chapter IV
RIGHTS AND RESPONSIBILITIES OF PRIVATE MEDICAL PRACTITIONERS
Apart from the rights and obligations prescribed in Chapter III of the Ordinance on private practice of medicine and pharmacy and Article 16 of the Government’s Decree No. 06/CP of January 29, 1994 detailing a number of articles of the Ordinance on private practice of medicine and pharmacy, the private medical practitioners shall have the following rights and obligations:
Article 27.-
1. Rights:
- The private hospitals are allowed to organize their own drug stores, but the procedures therefor must comply with the provisions of law.
- The private medical practitioners are allowed to take long-term study courses according to the State’s regulations on enrolment in order to raise their professional skills; and to participate regularly in professional fostering activities of the Health Service. The medical practitioners may attend refresher training courses to update their knowledge, particularly about dangerous epidemics (malaria, cholera, typhoid, HIV/AID…). The provincial/municipal Health Services shall have to coordinate with the provincial/municipal Medicine and Pharmacy Society in organizing training courses to raise the professional skills of the medical practitioners and provide them with update medical knowledge.
- Individuals and units that have merits in serving the patients shall be worthily commended and rewarded.
2. Responsibilities:
- To spare 3% of the hospital beds for poor people; other forms of private medical practice must organize medical examination for poor people free of charge.
- To hang up proper signboards, post up the hospital fee index and detailed scope of professional practice; to strictly comply with the permitted scope of professional practice and the approved hospital fees.
+ The private hospitals and medical examination and treatment establishments set up under the Law on Private Enterprises or the Law on Companies shall have to draw up the hospital fee tables and report them to the Ministry of Health for approval.
+ Various forms of private medical establishments shall have to draw up the hospital fee tables and report them to the provincial-level Health Services for approval.
- To have the medicine cupboards as prescribed; not to make prescription and sell drugs at the same time; not to prescribe the use of new medicines or the application of new techniques and equipment, that have not yet been permitted for circulation.
- Private medical establishments shall have to participate in epidemics prevention and combat and participate in the national medical programs. To forbid the sale of drugs and/or instruments of the programs (free of charge and with the State subsidies) for personal profits.
- Private medical establishments shall have to sign contracts with State-run medical institutions for technical support and transfer of patients when so requested.
Chapter V
MANAGEMENT OF PRIVATE MEDICAL PRACTICE
Article 28.-
1. The provincial-level Health Services shall act as the bodies assisting the provincial People’s Committees to perform their function of State management over the private medical practice, which must have sections or officials in charge of monitoring and managing the private medical practice. In such big cities as Hanoi, Ho Chi Minh City, etc., the municipal Health Services shall have to report to the municipal People’s Committees which shall further report to the Ministry of Health and the Government Commission for Organization and Personnel for permission to retain the already set-up sections for management of private medical practice of the Health Services with a view to helping the Health Service directors to manage the private medical practice in their respective localities.
2. The district Health Centers may appoint full-time or part-time officials in charge of monitoring and directly managing the private medical establishments in the localities, depending on their respective situation.
3. The commune-level Health Stations shall help the commune/ward People’s Committees in monitoring and creating favorable conditions for private medical establishments to bring into full play their effect in serving the people’s health, in primary healthcare as well as in implementing health programs.
Article 29.-
1. The provincial-level Health Services’ periodical reports sent to the Ministry of Health should contain sections on management of the private medical practice in their respective localities.
2 Annually, the provincial-level Health Services shall send their reports on private medical practice to the Ministry of Health.
3. The private hospitals and the medical examination and treatment establishments set up under the Law on Private Enterprises or the Law on Companies shall have to periodically report to the Ministry of Health.
Chapter VI
EXAMINATION, INSPECTION AND HANDLING OF VIOLATIONS
Article 30.- The Ministry of Health and the provincial-level Health Services shall organize regular or irregular inspection of the compliance with the provisions of law on private medical practice. Organizations and individuals engaged in private medical practice (including foreign-invested establishments) shall have to subject to and create favorable conditions for the examination and inspection and their establishments.
Article 31.- Handling of violations
Organizations and individuals engaged in private medical practice (including foreign invested establishments) that breach laws, violate regulations of this Circular or violate regulations on medical operation and techniques shall, depending on the seriousness of their violations, be administratively sanctioned according to the provisions of the Government’s Decree No. 46/CP of August 6, 1998 stipulating sanctions against administrative violations in the State management over health activities or examined for penal liabilities, and compensate for damage as prescribed by law.
Chapter VII
IMPLEMENTATION PROVISIONS
Article 32.- This Circular takes effect 15 days after its signing for promulgation and replaces Circular No. 07/BYT-TT of April 30, 1994 of the Minister of Health, guiding the implementation of the Ordinance on Private Practice of Medicine and Pharmacy and the Government’s Decree No. 06/CP of January 29, 1994 detailing a number of articles of the Ordinance on the Private Practice of Medicine and Pharmacy in the field of medical practice.
|
FOR THE MINISTER OF HEALTH |