Nội dung toàn văn Decision No. 1125/QD-BYT 2021 guidelines for the care of COVID-19 patients in healthcare establishments
|
MINISTRY OF HEALTH |
SOCIALIST REPUBLIC OF VIETNAM |
|
No. 1125/QD-BYT |
Hanoi, February 08, 2021 |
DECISION
ON GUIDELINES FOR CARE OF COVID-19 PATIENTS IN HEALTHCARE ESTABLISHMENTS
MINISTER OF HEALTH
Pursuant to the Government’s Decree No. 75/2017/ND-CP dated June 20, 2017 on functions, duties, powers and organizational structure of the Ministry of Health; at the request of Medical Services Administration, Ministry of Health,
HEREBY DECIDES:
Article 1. Promulgated together with this Decision are the guidelines for the care of COVID-19 patients in healthcare establishments.
Article 2. This Decision takes effect from the date on which it is signed.
Article 3. Head of Office of the Ministry of Health; Chief Inspector of the Ministry of Health; heads of departments of the Ministry of Health; Directors of Departments of Health; directors of hospitals and institutes with hospital beds affiliated to the Ministry of Health; heads of health units of other ministries and central authorities; and heads of relevant units shall implement this Decision./.
|
|
P.P. THE MINISTER |
GUIDELINES
CARE OF COVID-19 PATIENTS AT HEALTHCARE ESTABLISHMENTS
(Enclosed with Decision No. 1125/QD-BYT dated February 08, 2021 by Minister of Health)
OVERVIEW ON SARS-COV-2
I. Overview
Coronaviruses (CoV) are a virus family capable of animal-to-human transmission, resulting in illness ranging from the common cold to severe and life-threatening conditions such as the 2002 severe acute respiratory syndrome (SARS- CoV) and 2012 Middle East respiratory syndrome (MERS-CoV). In December 2019, a new strain of coronavirus (SARS-CoV-2) was confirmed as the cause of an outbreak of acute respiratory infection (COVID-19) in Wuhan city (Hubei, China), which has spread to all of China and almost all countries around the world. On 11/3/2020, the World Health Organization (WHO) declared COVID-19 a pandemic. Besides animal-to-human transmission, SARS- CoV-2 can be spread between humans, mostly through respiratory droplets and contact. The virus can also be transmitted via aerosols, especially in healthcare establishments, crowded places and enclosed spaces.
After the first case was confirmed in China on 08/12/2019, as of 02/02/2021, more than 1 year into the pandemic, the world records 102.626.724 cases and 2.216.279 deaths in more than 200 countries and territories. In Vietnam, as of 02/02/2021, there are 1. 851 cases and 35 deaths.
COVID-19 has diverse clinical manifestations, ranging from asymptomatic infection to severe illness such as severe pneumonia, respiratory failure, septic shock, multiorgan dysfunction and death, especially in the elderly and those with chronic diseases or immunodeficiency.
As of now, there is no medication for the disease. Vaccination against COVID-19 has recently started in some countries, which is facing multiple issues, thus, proactive precautions such as the use of face masks, use of personal protective equipment (PPE) in appropriate situations; hand hygiene; surface hygiene; keeping safe distance, avoiding gatherings, etc. are of most importance to COVID-19 prevention.
II. Diagnosis
1. Definition of COVID-19 cases
1.1. Suspected cases:
A suspected case involves:
A. A patient who has fever and/or acute respiratory disease that cannot be attributed to other causes.
B. A patient who has any respiratory symptom AND has traveled to/through/from or stayed in a COVID-19 infected epidemiological zone* in the 14 days prior to symptom onset OR has had close contact (**) with a suspected or confirmed COVID-19 case in the 14 days prior to symptom onset.
* Epidemiological zone: a country or territory recording domestically-transmitted COVID-19 cases or an active epidemic hotspot in Vietnam per the interim guidelines for COVID-19 monitoring and prevention promulgated by the Ministry of Health and updated by General Department of Preventive Medicine.
** Close contact includes:
- Contact at healthcare establishments, including direct care of a COVID-19 case; working with a health care worker infected with COVID-19; visiting a COVID-19 case or staying in the same room with a COVID-19 case.
- Direct contact within less than or equal to 2 meters with a suspected or confirmed COVID-19 case during period of illness.
- Living in the same house as a suspected or confirmed COVID-19 case during period of illness.
- Working with a confirmed or suspected COVID-19 case in the same team or office during period of illness.
- Being in a tourist group, business team, group of friends, etc. with a confirmed or suspected COVID-19 case during period of illness.
- Traveling in the same vehicle (sitting on the same row or within two rows in front of or behind) with a suspected or confirmed COVID-19 case during period of illness.
1.2. Confirmed cases
Confirmed cases are suspected cases or any person testing positive for SARS-CoV-2 confirmed by testing facilities permitted to perform such testing by the Ministry of Health.
III. Symptoms
1. Clinical symptoms
- Incubation period: from 2 to 14 days, from 5 to 7 days on average.
- Onset: common symptoms include fever, dry cough, fatigue and muscle pain. Some may experience throat pain, stuffy nose, runny nose, headache, productive cough, vomiting and diarrhea.
- Development:
+ Most patients (more than 80%) have only mild fever and fatigue without pneumonia and usually recover after about 1 week. However, some cases do not develop any clinical symptom.
+ About 14% of patients develop serious complications such as pneumonia or severe pneumonia and require hospitalization; about 5% of patients need to be admitted to intensive care units for treatment of acute respiratory manifestations (rapid breathing, dyspnea, cyanosis, etc.), acute respiratory distress syndrome (ARDS), septic shock, organ dysfunction, including kidney injury and heart muscle injury, leading to death.
+ It takes an average of 7 to 8 days after symptom onset for serious complications to develop.
+ Death is more common in the elderly and persons with immunodeficiency and chronic diseases.
- Recovery period: from 7 to 10 days after the period of illness; if without ARDS, patients will no longer have fever, clinical signs will gradually disappear and they will make a recovery.
- There is no evidence of different clinical manifestations of COVID-19 in pregnant women.
- In pediatric patients, most of them have milder clinical manifestations compared to adult patients or no symptom. Common signs include fever and coughing or manifestations of pneumonia. However, some pediatric patients suffer from multiorgan inflammation, fever; hyperemic eye or erythema, or swelling of the oral mucosa, hands, feet; circulatory failure; manifestations of heart dysfunction and high cardiac enzymes level; digestive disorders; coagulation disorders and high inflammatory marker levels.
2. Paraclinical tests
Non-specific blood tests and biochemical tests:
- Leukocyte count is normal or decreases; lymphocyte count usually decreases, especially in severe cases.
- C-reactive protein (CRP) level is normal or increases, procalcitonin (PCT) level is usually normal or increases slightly. ALT, AST, CK, LDH may increase slightly in some cases.
- Severe cases may develop organ dysfunction, coagulation disorders, D-dimer level increase, electrolyte and acid-base imbalance.
3. Lung X-ray and CT scan
- In the early phase of the disease or if there is only upper respiratory tract infection, radiographs look normal.
- When pneumonia develops, there are usually signs of bilateral interstitial pneumonia or diffuse ground-glass opacity in peripheral or lower areas of the lungs. The injury can progress rapidly in ARDS. Signs of cavity formation, pneumothorax or pleural effusions are rare.
4. Confirmatory testing
- SARS-CoV-2 may be detected via Real time RT-PCR or next-generation sequencing.
IV. Clinical form classification
Clinical forms of COVID-19:
1. Asymptomatic form
2. Mild cases: acute upper respiratory tract infection
- There are non-specific clinical symptoms such as fever, dry cough, throat pain, stuffy nose, fatigue, headache and muscle pain.
- There are no signs of pneumonia or oxygen deprivation.
3. Moderate cases: pneumonia
- Adult and old pediatric patients: pneumonia (fever, cough, dyspnea, rapid breathing) and no sign of severe pneumonia.
- Young pediatric patients: have cough or dyspnea and rapid breathing (rapid breathing refers to a respiratory rate of ≥ 60 breaths/minute in children under 2 months of age; ≥ 50 breaths/minute in children from 2 to 11 months of age; ≥ 40 breaths/minute in children from 1 to 5 years of age) and no signs of severe pneumonia.
- Interstitial pneumonia or complications is/are detected via lung X-ray, ultrasound or CT scans.
4. Severe cases: severe pneumonia
- Adult and older pediatric patients: have fever or are suspected of respiratory infection, accompanied by any of the following signs: respiratory rate of > 30 breaths/minute, severe dyspnea.
- Young pediatric patients: have cough or dyspnea and at least one of the following signs: cyanosis or SpO2 < 90%; severe respiratory failure (grunting noises when breathing, retractions);
+ Or the child is diagnosed with pneumonia and has any of the following severe signs: inability to drink/nurse; altered level of consciousness (lethargic or comatose); convulsions. Other pneumonia signs such as retractions or rapid breathing may be present (with the abovementioned respiratory rate).
- Diagnosis is made based on clinical signs; complications are detected via lung X-ray.
5. Critical cases
5.1. Acute respiratory distress syndrome (ARDS)
- Onset: respiratory symptoms appear or worsen within one week starting from onset of clinical symptoms.
- Lung X-rays, CT scans or ultrasound images: ground-glass opacity in both lungs that is not caused by pleural effusion, lobar atelectasis or lung nodules.
- Pneumochysis is not caused by heart failure or fluid overload. Subjective assessment (heart ultrasound) is needed to exclude pneumochysis caused by hydrostatic pressure if there are no risk factors.
- Hypoxemia in adult patients: classification is done based on PaO2/FiO2 (P/F) ratio and SpO2/FiO2 (S/F) ratio if PaO2 value is unavailable:
- Hypoxemia in pediatric patients: classification is done based on IO or OSI value for patients on invasive ventilation and PaO2/FiO2 or SpO2/FiO2 for patients on CPAP or non-invasive ventilation.
5.2. Sepsis
- In adult patients: there are signs of organ dysfunction:
+ Altered level of consciousness: somnolence, stupor, coma
+ Dyspnea or rapid breathing, low oxygen saturation level
+ Fast heart rate, weak pulse, cold extremities, or low blood pressure, livedo reticularis
+ Low urine output or no urine output
+ Laboratory tests show coagulation disorders, thrombocytopenia, acidosis, high lactate level, high bilirubine level, etc.
- Pediatric patients: when sepsis is suspected or confirmed and at least 2 criteria for systemic inflammatory response syndrome (SIRS) are met, one of which must be change to body temperature or abnormal leukocyte count.
5.3. Septic shock
- In adult patients: prolonged low blood pressure despite volume resuscitation, use vasoactive drugs to maintain mean arterial pressure (MAP) at ≥65 mmHg and serum lactate levels at >2 mmol/L.
- In pediatric patients: septic shock is confirmed upon the presence of:
+ Low blood pressure.
+ Or 2-3 of the following signs: altered level of consciousness, fast or slow heart rate; or warm vasodilation with bounding pulses; rapid breathing; mottled skin or petechial or purpuric rash; increased lactate; oliguria; hyperthermia or hypothermia.
5.4. Other severe-critical complications: lung infarction, stroke, delirium. They require close monitoring, diagnostic testing upon suspicion and suitable treatments.
V. Treatment and care
1. General treatment rules
- Classify patients and identify the location where a patient will receive treatment depending on level of severity:
+ Suspected cases shall be examined, monitored and isolated in a separate area in healthcare establishments, and have their samples collected properly for confirmatory testing.
+ Confirmed cases must be monitored and treated in complete isolation in designated establishments.
+ Mild cases shall be treated in isolation areas of normal departments.
+ Severe cases shall be treated in isolated emergency rooms of departments or intensive care units.
+ Severe-critical cases shall be treated in intensive care units.
- As there is no known effective cure, treatment mostly involves supportive care and symptom treatment.
- Treatments shall be individualized for each case, especially for severe-critical cases.
- Severe conditions and complications must be monitored, detected and handled promptly.
2. General monitoring, care and treatment measures
- Patients shall be on bed rest, patient rooms must be well ventilated, air filtration systems or other patient room disinfection measures such as ultraviolet light (if any) may be used.
- Clean the nose and throat, can keep the nose moisturized with saline, gargle with regular mouth wash.
- Keep the body warm.
- Drink enough water, ensure fluid and electrolyte balances.
- Be careful when administering IV fluids to pneumonia patients who have no signs of shock.
- Ensure a balanced diet, improve the body’s condition and administer vitamin supplements if necessary. For severe-critical cases, follow nutrition recommendations of Vietnam National Association of Emergency, Intensive Care Medicine and Clinical Toxicology.
- Reduce high fever.
- Reduce cough using common cough medications if necessary.
- Evaluate, treat and give a prognosis of comorbid chronic conditions (if any).
- Give advice and encouragement to patients.
- Closely monitor clinical signs and progress of lung damage on lung X-ray films and/or CT scans.
- Treating establishments shall be equipped with minimum emergency aid equipment and tools such as pulse oximeters, oxygen supply systems/tanks, oxygen-delivering interfaces (nasal cannula, simple face mask, and mask with reservoir bag), bag valve masks, and endotracheal intubation equipment for different age groups.
3. Treatment of respiratory failure
3.1. Oxygen therapy and monitoring
- Give supplemental oxygen therapy immediately to patients with SARI and respiratory failure, hypoxaemia or shock.
- Closely monitor each patient's condition to detect worsening signs or poor response to oxygen therapy for timely handling.
3.2. Treatment of critical respiratory failure and ARDS
- When low flow oxygen therapy is not effective against hypoxemia, SpO2 ≤ 92%, or/and there is labored breathing, consider administration of high flow nasal oxygen, CPAP, or BiPAP.
- Do not put patients with hemodynamic disorders, multiorgan dysfunction and altered level of consciousness on non-invasive ventilators.
- Closely monitor patients to detect poor response for timely handling. If non-invasive breathing support is not effective against oxygen deprivation, administer endotracheal intubation and invasive ventilation.
- Endotracheal intubation should be performed by an experienced worker using airborne precautions.
- Implement breathing support regimens for ARDS in adults and children.
- Strictly control fluid balance, avoid fluid overload, especially when not performing volume resuscitation.
- In case of severe and prolonged oxygen deprivation not responding to common therapies, consider indication and use of extracorporeal membrane oxygenation (ECMO) techniques on each case where qualified to perform such techniques.
- As ECMO can only be performed at some large healthcare establishments, upon consideration of ECMO indication, the treating establishment should contact a qualified establishment, transport the patient early and follow the patient transport procedure from the Ministry of Health.
4. Treatment of septic shock
Apply treatment regimens for septic shock in adult and pediatric patients.
5. Supportive care for organ dysfunction
Supportive care shall be provided as appropriate to each patient’s condition.
- Supportive care for kidney dysfunction:
- Supportive care for liver dysfunction: in case of liver failure
- Treatment of coagulation disorders: transfuse fresh plasma, platelets and coagulation factors if necessary.
6. Other treatment measures
- Antibiotics
- Antiviral drugs
- Systemic corticosteroids
- Hemofiltration
- Intravenous immunoglobulin (IVIG)
- Interferons
- Pulmonary rehabilitation
- Detection and handling of neurological and mental manifestations
7. Complication prevention
For severe cases receiving treatment in intensive care units, take preventive measures against the following common complications:
- Ventilator-associated pneumonia
- Venous thrombosis prevention
- Central line-associated bloodstream infection
- Pressure ulcers
- Stress-induced stomach ulcers and gastrointestinal hemorrhage
- Intensive care unit acquired muscle weakness
VI. Discharge criteria
1. A COVID-19 patient may be discharged when all of the following criteria are satisfied:
- No fever for at least 3 days.
- Improved clinical symptoms, good general condition, stable vital signs, normal organ functions, normal blood test results and better lung X-rays.
- 03 samples (collected at least 1 day apart) testing negative for SARS-CoV-2 via realtime RT-PCR.
2. Post-discharge monitoring
The patient shall self-quarantine under the supervision of grassroots health unit and local CDC for 14 days and take temperature twice a day; if their temperature is higher than 38oC in two consecutive checks or there is any other abnormal sign, they must visit a healthcare establishment for examination immediately.
MANAGEMENT OF COVID-19 CASES
1. Receipt and screening of COVID-19 cases
As SARS-CoV-2 is highly contagious, screening, early detection and timely treatment are crucial. Prompt quarantine and precautions against transmission must be applied to suspected cases.
1.1. General rules
- Healthcare establishments shall formulate plans for prompt detection, classification, screening and management of confirmed or suspected cases, including patients, patients' families, visitors and healthcare workers, upon their arrival at these establishments. After arriving at these establishments, persons with respiratory tract infection symptoms (cough, fever, runny nose, throat pain, chest tightness, dyspnea, body aches) and persons having epidemiological factors (traveling from infected areas, having contact with confirmed or at-risk cases, etc.) shall receive instructions and be screened and examined separately. Healthcare establishments not receiving COVID-19 patients for treatment shall establish referral procedures for suspected cases.
- Healthcare establishments shall formulate plans for screening of inpatients, patients’ families, visitors and healthcare workers, especially for departments facing high risk such as kidney dialysis, intensive care, infection, respiratory medicine, oncology, etc.
- Take precautions and control contamination seriously (standard precautions and transmission-based precautions).
1.2. Classification and receipt of visiting patients
1.2.1. For establishments with 2 or more gates
Step 1. At establishment’s entrance (initial screening)
- Dedicate only one gate to receipt and service of persons having respiratory tract infection symptoms. Place a sign reading “Gate for persons having cough, fever, runny nose, throat pain, chest tightness, breathing difficulty and body aches and contact with confirmed or suspected COVID-19 cases” at this gate. Place another sign reading “Persons having cough, fever, runny nose, throat pain, chest tightness, breathing difficulty and body aches please enter via gate ..." at the other gates.
- At the dedicated gate, place a sign with colored lighting (e.g., LED light signs, box signs with lights inside or requiring lighting) for reading at night.
- Similar instruction signs, information on hotlines, etc. shall be placed at noticeable locations outside of the gates.
- Place the parking lot outside of the gates or next to the gates. Provide sufficient training in COVID-19 prevention for security guards and parking lot staff.
- Place a health declaration and registration table at a well-ventilated location next to the establishment’s gate or in the lobby. Remind patients and their families to wear face masks and provide face masks for those not having them. Equip health declaration and registration tables with alcohol-based hand sanitizer.
Step 2. Route to screening rooms
- Dedicate a route from the gate to the screening room using red/ yellow ropes (may be reflective). Place a sign instructing persons with symptoms to use only this route.
- Assign at least 1 specialized patient transport vehicle (for long distance) to transport confirmed or suspected COVID-19 cases. This vehicle shall be parked in a separate area denoted by a sign, not be used to transport other patients and must be disinfected after each use.
Note: the route shall not go through other departments and rooms, avoid going down corridors. Place screening rooms as near health declaration and registration tables as possible.
Step 3. Screening rooms
- Place screening rooms at well-ventilated locations separate from other departments and rooms.
- Each screening room shall have only one examination table. Do not examine two people in one screening room at the same time.
- Examination tables shall be fully supplied with COVID-19 prevention equipment. Each room shall have only one examination table.
Step 4. Post-screening classification
After screening a person, if it is confirmed that the person has no epidemiological factor or clinical symptom related to COVID-19, direct the person to the normal examination area. Vice versa, the normal examination area shall transfer all persons with suspected factors (epidemiological factors and/or clinical symptoms) to screening rooms.
Step 5. Transfer to another establishment or isolation area for COVID-19 treatment
- After screening, if a patient is suspected to have contracted SARS-CoV-2, the establishment shall transport the patient to one of the two following locations:
a) Temporary isolation room in the establishment: transport the patient to a temporary isolation room if the establishment is not designated for COVID-19 treatment. The establishment shall contact the preventive medicine center/ CDC and the nearest hospital designated for COVID-19 treatment to transfer the patient there and prevent infection during the transfer process.
- Establishments shall not transfer patients by themselves. They must contact their supervisory bodies and hospitals at higher level immediately for guidance.
b) Isolation areas for COVID-19 treatment:
- Hospitals designated for COVID-19 treatment shall prepare isolation areas to receive patients. Isolation areas shall conform to guidelines of the Ministry of Health and accommodated the following three groups of patients separately:
+ Suspected cases
+ Mild cases
+ Severe cases
Collect samples (at establishments or another location)
If collecting a sample for SARS-CoV-2 testing is indicated, collect the sample in the isolation area or temporary isolation room. Establishments may collect samples in respiratory examination rooms depending on their actual capacity. Establishments shall contact CDC/ preventive medicine unit for sample collection or collect samples themselves if they are permitted to perform SARS-CoV-2 testing by the Ministry of Health.
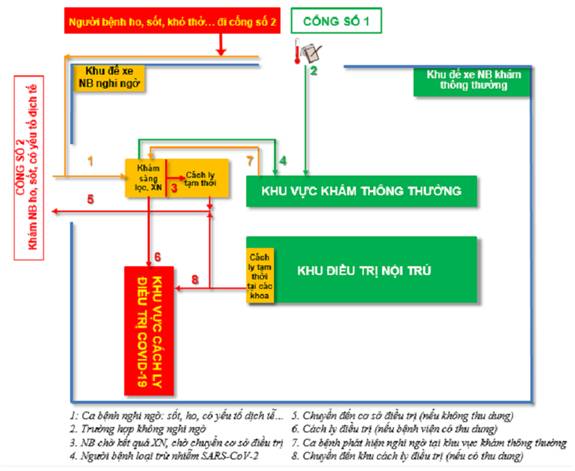
Picture 1: Diagram of classification and screening for establishments with multiple gates
1.2.2. For establishments with 2 or more gates
Adhere to the guidelines for hospitals with 2 gates and the following points:
- Place instruction signs from the gate to the registration and classification tables/ rooms.
- Registration and classification tables/ rooms shall be placed next to the gate or in the yard or main lobby as close to the gates as possible. Do not place registration and classification tables/ rooms inside the main buildings or near departments or rooms to minimize infection risk.
- Screening rooms shall be placed next to registration and classification tables/ rooms (within 10m from the gate).
Note: if a COVID-19 case is found in an inpatient department, the patient must be placed under temporary isolation in the department's temporary isolation room.
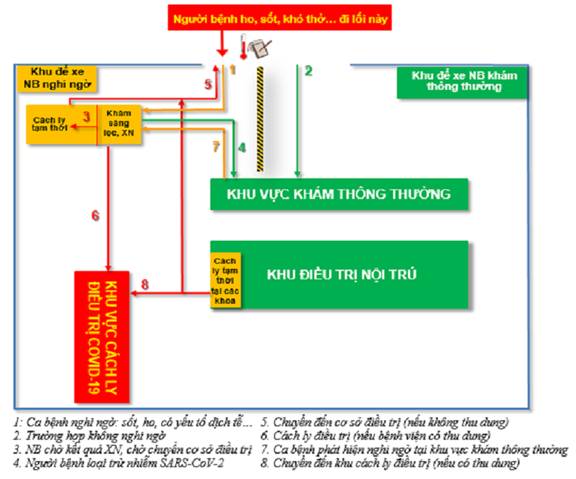
Picture 2: Diagram of classification and screening for establishments with one gate
- During an epidemic, instructional signs shall be affixed at entrances and in examination rooms to instruct patients with fever or cough and their families to visit the screening area immediately, preventing them from visiting other areas.
- Instruct patients and their families to wear face masks, avoid having contact with other people and practice hand hygiene as well as respiratory hygiene properly.
- Any family member accompanying a confirmed or suspected case shall be considered to have been exposed to SARS-CoV-2 and must be monitored for the prescribed period to faciliate early diagnosis of COVID-19.
- Persons in charge of transporting confirmed or suspected cases must wear PPE and use specialized vehicles. Contaminated items, transport vehicles, discarded items and waste associated with these persons shall be collected and handled according to regulations.
2. Organization of COVID-19 treatment areas
- A treatment area shall have the following rooms: examination room, laboratory, treatment monitoring room and cardiopulmonary resuscitation room.
- The building layout and operational process must meet standards for hospital isolation.
- If possible, place confirmed cases in negative pressure rooms.
- Entry to isolated treatment areas must be controlled strictly.
3. Patient arrangement
- Suspected and confirmed cases must be placed in separate areas in a department and not stay in the same room.
- Serious cases shall be placed in special care rooms (negative pressure if possible) in isolation areas or isolation rooms fully equipped with ventilators and blood filters.
- Mild cases shall be placed in separate rooms. If this is not possible, they may stay in the same room.
- Suspected cases must be isolated in single-occupancy rooms or placed in the same room with their beds at least 1-2 meters apart.
- All patient activities must be limited to isolation areas.
4. Workforce preparation
- Healthcare establishments shall prepare resources and workforce plans for receipt and treatment of COVID-19 cases during epidemics, minimize mortality and control infection in healthcare establishments and communities.
- Depending on current capacity of clinical and paraclinical departments/ units (hereinafter referred to as “units”) compared to last year, healthcare establishments shall classify these units into at least 3 operating groups:
+ Group working from home
+ Group working in treating departments
+ Group working in screening areas, anterooms and areas where COVID-19 cases are treated.
- Formulate detailed plans for workforce mobilization according to epidemic situation and possible quarantine scenarios, avoiding mobilizing large workforce at the start.
- All healthcare workers must be ready to work in unfamiliar situations such as working with new teams in new situations and being led by members of emergency and infection teams.
- Set targets at the beginning: minimize risks and complications for patients; minimize cross-contamination to healthcare workers. Care may not be perfectly and promptly provided due to lack of PPE and prolonged fatigue and stress in healthcare workers.
- Each care group shall work no more than 1 shift/ day in COVID-19 treatment areas.
- Before end of shift, healthcare workers must change out of their PPE and perform necessary personal hygiene to prevent infection from their work.
4. Health monitoring for healthcare workers
- Frontline workers in isolated treatment areas, including doctors, nurses, technicians and orderlies, must live in isolated areas and shall not leave these areas without permission.
- Healthcare workers need to have a nutritious diet to boost their immune systems.
- Monitor and record the health condition of all frontline healthcare workers, including temperature and respiratory symptoms. If a worker develops any symptom such as fever or cough, they must be isolated immediately and tested for the virus.
- Nurses directly taking care of confirmed cases require assistance and mental preparation to work and care for an increasing number of patients as well as risk of cross-contamination from patients.
- When frontline healthcare workers have completed their duties in isolated treatment areas and return to their normal life, they should be tested for SARS-CoV-2. If testing negative, they need to undergo quarantine in a separate area according to regulations before returning home.
5. Preparation of medical equipment and materials and PPE
- Draw up lists of names and quantities of medical devices (premium ventilators, invasive/ non-invasive ventilators, electric syringe pumps, infusion pumps, monitors, lights for endotracheal intubation, etc.) and medical consumables (PPE, alcohol-based hand sanitizer, etc.) to be equipped for screening rooms, isolation rooms and intensive care units as appropriate to the size and scope of service of each establishment for each COVID-19 epidemic stage.
- Decide PPE quota for each at-risk area (low, moderate or high risk) according to guidelines of the Ministry of Health.
- Determine levels of PPE necessity as suitable. All healthcare workers, patients’ families, visitors (if any) and persons having contact with confirmed or suspected COVID-19 cases or samples thereof shall be provided with recommended PPE (see Table 1).
- Cooperate with departments in stockpiling essential materials to ensure operations of healthcare establishments and units in charge of procurement shall promptly formulate plans to stockpile essential goods according to the epidemic’s progress and commitment on delivery time of manufacturers.
- All workers at healthcare establishments must wear face masks.
Table 1. Selection and use of COVID-19 personal protective equipment by location, user and professional operation at healthcare establishments
|
Location |
User |
Professional operation |
Level of COVID-19 PPE |
|
Screening room |
Healthcare workers |
Consultation with and physical examination of patients with no respiratory symptoms |
Level 3 or higher |
|
Healthcare workers |
Consultation with and physical examination of patients with respiratory symptoms |
Level 4 |
|
|
Cleaning staff |
After and during consultations and physical examination of patients with respiratory symptoms |
Level 3 or higher |
|
|
Healthcare workers |
Preliminary screening with no direct contact |
Level 2 |
|
|
Emergency department receiving patients with undetermined COVID-19 transmission risks |
Healthcare workers |
Procedures potentially capable of generating aerosols or surgeries |
Level 4 |
|
Healthcare workers |
All activities |
Level 3 |
|
|
Isolation areas |
Healthcare workers |
Direct patient care without aerosol generation |
Level 3 or higher |
|
Procedures potentially capable of generating aerosols or surgeries |
Level 4 |
||
|
Cleaning staff |
Entering patient rooms |
Level 3 or higher |
|
|
Laboratories testing samples of confirmed or suspected COVID-19 cases |
Healthcare workers |
All activities |
Level 4 |
|
Transport of COVID-19 cases |
All staff, including healthcare workers |
All activities |
Level 3 or higher |
|
Other areas with patient presence in isolation areas |
All staff, including healthcare workers |
Any activity without contact with patients |
Level 3 |
|
Departments of infection control |
Handlers of waste at healthcare establishments |
Collection and handling of waste at healthcare establishments |
Level 3 or higher |
|
Morgues |
All staff, including healthcare workers |
All activities |
Level 4 |
6. Formulation of COVID-19-related regular procedures
Healthcare establishments shall look for guidelines of the Ministry of Health or formulate guidelines and procedures for healthcare workers to ensure safety in the care of COVID-19 patients.
- Procedures for patient receipt, classification and screening
- Guidelines and procedures for putting on and removing PPE
- Collection of COVID-19 samples, preservation, packing and transport of samples from confirmed or suspected COVID-19 cases
- Procedures for disinfection of COVID-19 screening and isolation areas
- Procedures for handling of bodily fluids and blood of confirmed or suspected COVID-19 cases
- Procedures for handling of COVID-19-related biomedical waste
- Procedures for handling of exposure to SARS-CoV-2 for healthcare workers
- Procedures for handling of remains of confirmed or suspected COVID-19 cases
- Procedures for handling of medical equipment and textile products
7. Training
- Establish a COVID-19 training committee, which shall take charge of compiling training materials and providing training for the whole healthcare establishment.
- Standardize all procedures (making video clips) to facilitate online training and E-learning.
- Prioritize training for the following 3 groups:
+ Core group (nurses and medical technicians working in screening, emergency and respiratory medicine areas), which shall receive training in advanced skills and knowledge about care of ventilated severe COVID-19 cases, ECMO, etc.
+ Extended group (nurses of clinical departments participating in treatment of mild to moderate COVID-19 cases in case of overload in emergency departments and specialized areas for COVID-19 cases), which shall receive training in basic skills and knowledge and general rules in care of confirmed or suspected cases, precautions (use of PPE, negative pressure rooms, etc.), and educating patients and their families about health matters.
+ Peripheral group (orderlies, security guards, cleaning staff and other persons), which shall receive training in infection prevention, rules for approaching confirmed or suspected cases and basic precautions.
- Drills: organize drills to inspect, assess and take note of areas of improvement to amend and complete COVID-19 prevention and control plans of healthcare establishments.
8. Inspection and supervision
- Establish a team in charge of inspecting compliance with administrative regulations on COVID-19 prevention and control in each healthcare establishment.
- The nursing department shall cooperate with the department of infection control, general planning department, head nurses of clinical departments and head technicians of paraclinical departments in inspecting and supervising compliance with regulations on COVID-19 prevention and control.
9. Provision of comprehensive care to suspected or confirmed COVID-19 cases
- Monitor vital signs of patients continuously, especially changes in consciousness, respiratory rate and oxygen saturation. Observe symptoms such as cough, sputum, chest pain, dyspnea and cyanosis. Monitor arterial blood gas analysis closely. Promptly recognize any worsening condition to adjust oxygen supply or take other emergency measures.
- Pay attention to ventilator associated lung injury (VALI) with higher positive end-expiratory pressure (PEEP) and high pressure support. Closely monitor changes in airway pressure, tidal volume and respiratory rate.
- Aspiration prevention:
+ Monitor gastroparesis. Evaluate gastroparesis every 4 hours. Replace fluid removed if remaining gastric volume is under 100 ml; otherwise, inform the in-charge doctor.
+ Prevent aspiration during patient transport: before transporting the patient, stop feeding via nasogastric tube, remove gastric residue and connect gastric tube to a negative pressure bag. Throughout transport, elevate the patient’s head to 30 degrees.
+ Prevent aspiration for HFNC: check humidity every 4 hours to prevent overly high or low humidity. Promptly remove water in the cannula to prevent cough and aspiration induced by condensation. Keep the nasal cannula higher than the machine and tube. Promptly remove condensation in the system.
- Adopt strategies for prevention of catheter-related sepsis and catheter-related urinary tract infection.
- Prevent skin damage due to pressure, including medical device-related pressure injuries, incontinence-associated dermatitis and medical adhesive-related skin injuries.
- Identify patients with high fall risk and take precautions.
- Assess all patients with venous thromboembolism risk to identify those at high risk and take precautions. Monitor coagulation, Ddimer level and clinical manifestations related to VTE.
- Assist patients who are weak, have breathing difficulty or have significant oxygenation index fluctuation with eating and drinking. Increase monitoring of oxygenation index of these patients during their meals. Give tube feeding for those who cannot eat. In each shift, adjust feeding volume and speed according to patient’s intake capacity.
PREVENTION OF INFECTION IN CARE OF COVID-19 CASES
1. Rules for infection prevention
- Apply standard precautions: all healthcare workers working in isolation areas shall wear sufficient PPE properly. This is the most important measure to protect healthcare workers from the disease.
- Take precautions against contact and droplet transmission in examination and care of confirmed or suspected COVID-19 cases.
- Take precautions against airborne transmission while performing aerosol generating procedures upon confirmed or suspected COVID-19 cases.
- All patients and healthcare workers in isolated treatment areas shall practice respiratory hygiene.
- Properly control ventilation and environmental hygiene in patient rooms, isolation areas, etc.
- Minimize moving patients. Prioritize bedside techniques (X-ray, ultrasound, etc.); if the patient must be moved, notify the destination and ask the patient to wear a medical mask during the move; use separate and predetermined ways to minimize exposure for healthcare workers and other patients.
- Do not let the family of isolated patients take care of them, excluding newborns and young children; families of suspected or confirmed cases must strictly adopt preventive measures.
- Patient care equipment shall be used once for each patient. If this requirement cannot be ensured, sanitize, disinfect and sterilize the equipment before using it on another patient.
2. Standard precautions are a set of basic precautions applied to all patients in healthcare establishments, regardless of their diagnosis, infection status and time of care, by treating all bodily fluids (excluding sweat) and excreta as potentially infectious. Standard precautions must be used in the care of all patients in healthcare establishments, regardless of their diagnosis and infection status.
3. Transmission-based precautions
3.1. Droplet precautions
Wear medical masks and goggles or face shields when in close contact with confirmed cases.
3.2. Contact precautions
- Wear clean gowns and shoe covers when visiting a patient’s room and remove them before exiting the anteroom. Do not let work clothing touch any environmental surface or other objects.
- Wear clean gloves while caring for patients, change gloves after coming into contact with feces, medical fluids, bodily fluids of patients, etc.
- Clean hands immediately using hand sanitizer.
3.3. Airborne precautions
- Wear gowns and respirator masks (e.g., N95).
- Use closed sputum suctioning equipment for patients on breathing support if sputum suctioning is indicated.
- Perform medical procedures in a single-occupancy room with a tightly shut door and safe ventilation. Negative pressure rooms are recommended.
- Ensure safe ventilation: natural ventilation, mechanical ventilation or mixed-mode ventilation may be used provided that the minimum ventilation rate is 12 ACH. Locate the exhaust system in a manner that allows air to be discharged close to the ground (10 - 15 cm above the ground) to empty areas and prevents contaminated air from recirculating.
4. Rules for respiratory hygiene
- Cover the mouth and nose with tissue papers when coughing and sneezing, and immediately discard used tissues in waste containers.
- If no tissue paper is available, cough into the elbow, DO NOT cough into the hand.
- Wash hands immediately after coming into contact with patients.
5. Control of isolation area environment
- Control of patient bed, floor, wall and corridor environments is an important precaution against the spread of SARS-CoV-2 with the following key areas:
- Patient receipt area, corridors and waiting rooms shall be well-ventilated and spacious.
- For patient rooms:
+ Negative pressure rooms are the optimal option.
+ In case negative pressure rooms are unavailable, employ mixed air or natural ventilation and ensure that the minimum ventilation rate is 12 ACH.
+ Aerosol generating procedures shall be performed in closed rooms with suitable ventilation (12 ACH).
- If there is no room meeting the abovementioned standards:
+ Perform the procedure in a room far away from other patients, which must be well-ventilated, located downwind and equipped with dual airflow windows opening out into empty areas.
+ An exhaust system may be used to discharge air to empty areas instead of corridors or adjacent rooms.
+ Environmental surfaces must be cleaned and disinfected with suitable and licensed disinfectants.
- Equipment, machinery, beds and cabinets shall be cleaned and disinfected at least twice a day and when necessary (when they are used for another patient or the current user is deceased, transferred or discharged) using suitable and licensed disinfectants.
Table 2. Chlorine-based disinfectants for COVID-19 prevention and control at healthcare establishments
|
Location and time |
Activated chlorine concentration |
Remark |
|
Surfaces of ordinary areas (floors, walls, objects) |
0,1% |
Minimum concentration of 0,1% for wiping or spraying (for hard to wipe surfaces) |
|
Surfaces of isolation areas |
0,1% |
|
|
Surfaces of equipment in isolation rooms |
0,1% |
Wiping or spraying (depending on location) |
|
Patient transport vehicles |
0,1% |
Minimum concentration of 0,1% for wiping or spraying (for hard to wipe surfaces) |
|
Spills of blood or other bodily fluids |
0,5% |
|
|
Excreta (urine, feces, vomit, fluids from suctioning, etc.) |
1,0% |
Add disinfectant to excreta in a ratio of 1 to 1 for at least 30 minutes |
|
Testing tables and equipment |
0,5% |
Refer to manufacturer’s guidelines |
|
Handling of remains |
0,1% |
Place the whole body in the first specialized bag and spray disinfectant over the bag. After moving out of the isolation room, place the first bag in another bag and spray disinfectant over this bag. |
|
Disinfect equipment, surfaces of operating tables, operating rooms and equipment involved in encoffinment and dissection of remains |
||
|
Patient’s tableware |
0,05% |
Soaking |
|
Textile items |
0,01%- 0,05% |
Depending on the state of the bloodstain or bodily fluid stain and type of fabric |
6. Use of PPE
- Infection usually occurs when PPE is taken off. Excluding goggles and face shields, which may be placed in basins containing a disinfectant solution for reuse, all PPE items must be discarded in specialized bags, transported by specialized vehicles and handled according to procedures for infectious waste handling.
- Place sufficiently large and understandable posters about PPE wearing and taking off at noticeable locations.
- Wear and take off PPE according to regulations at designated locations.
- PPE removal procedure is a reversal of the PPE wearing procedure.
- Besides use of PPE, surface and equipment disinfection, minimizing unnecessary contact with patients and surfaces and proper waste management are crucial to minimizing infection risk.
- Speak loudly, clearly and slowly when wearing face masks and masks. After hearing an instruction, repeat it to the speaker. Wear a name tag or affix a portrait onto the outside of the PPE for identification.
- Provide communications equipment such as cameras, phones, handheld transceivers, etc. inside and outside of isolation areas.
7. Prevention of infection in patient care
7.1. For patients receiving oxygen therapy
Ensure the “SAS” rule:
- Safe: safe for caregivers and patients.
- Accurate: avoid unreliable, unfamiliar or repetitive techniques.
- Swift: not hasty or late.
Healthcare workers face higher risk of infection when they directly take care of patients receiving oxygen therapy:
- Take safety measures to minimize contact or droplet COVID-19 transmission. When using HFNC, ensure that the nasal cannula is located correctly (completely placed inside the nostrils and secured to the patient’s head using a rubber band to minimize loss).
- Minimize infection in performance of aerosol generating procedures on suspected or confirmed COVID-19 cases. Aerosol generating procedures comprise airway suctioning, bronchial endoscopy, endotracheal intubation, tracheostomy and cardiopulmonary resuscitation, including non-invasive ventilation.
Perform these procedures in negative pressure rooms with at least 12 ACH. The patient shall stay in a separate room with natural ventilation.
- Healthcare workers who perform these procedures must wear waterproof long-sleeve gowns, non-sterile gloves (2 pairs), safety goggles (with temples), N95/FFP2 masks and face shields.
- Use closed sputum suctioning equipment.
- Avoid mask ventilation unless necessary and use the low pressure/ low volume technique. It is recommended to use the two-hand two-person V-E technique with the second person squeezing the bag.
- Endotracheal intubation of suspected or confirmed COVID-19 cases poses high risk to healthcare workers regardless of the clinical severity of the disease. Therefore, it is imperative to follow all necessary precautions; and practices recommended for special care and anesthesia teams.
- Prioritize early and planned endotracheal intubation instead of emergency endotracheal intubation to minimize infection risk.
- If possible, avoid bag-mask ventilation.
- Ensure the patient reaches the necessary level of sedation (no stimulation).
- Only essential healthcare workers may remain in the room.
- Ensure all necessary equipment and drugs are available in the room. Do not use trolleys.
7.2. For patients requiring surgery
- Prepare a plan to move the patient from the isolation area to the operating room and vice versa. Warn other people that the patient is suspected or confirmed to have contracted COVID-19 (using signage, labels, designated colors, etc.).
- The patient shall wear a medical mask and headwear, lie on a bed or stretcher or sit in a wheelchair and not talk during the move.
- Healthcare workers shall notify the operating room before the move to have it ready.
- Wear PPE and move the patient to the operating using the predetermined route. Avoid using the elevator.
- Promptly hand the patient over, go through the surgical safety checklist and move the patient directly into the operating room without staying in any other room.
- Do not take the patient’s medical record into the operating room; all post-surgery medical records shall be provided online, on temporary notes or via a board shown through the operating room’s window, which shall be copied and added to the patient’s medical record and signed by the responsible healthcare workers after the surgery in the administrative area after they have removed their PPE.
- The operating room: prioritize negative pressure operation rooms. If the operating room has positive pressure, turn the positive pressure system off if possible. A note informing about the COVID-19 patient must be posted on the operating room’s door.
- Minimize number of people present in the operating room. Only the anesthesiologist, anesthesiologist’s assistant, surgeon, surgeon’s assistant, surgical tech and communication staff member may stay in the operating room. Additional personnel may join depending on the situation.
- Select the most experienced doctors and personnel.
- Avoid opening the operating room’s door during the surgery. Communications between the operating room and the outside shall be done via handheld transceivers, phones, signals, etc. A person should stand at the door to pass on information where necessary.
- Do not replace any member of the surgical team throughout the surgery unless compulsory.
- Collect waste according to regulations.
- Carry out sterilization and disinfection according to regulations.
- Immediately sterilize the operating room and equipment used on the patient (endotracheal intubation light, mandrine, masks, ventilators and ventilator tubes, monitors, electric syringes, etc., replace PetCO2 monitor’s tubes and breathing filters).
- After the patient leaves the operating room, leave the room empty until 99,9% of its air has been replaced (e.g., an operating room with at least 15 ACH requires at least 28 minutes).
- After the surgery, clean and disinfect frequently touched surfaces at the anesthesia machine and anesthesia area using disinfectants. Consider using disposable covers (such as nylon covers) to prevent contamination of equipment and environmental surfaces.
Refer to the guidelines for prevention and control of SARS-CoV-2 infection at healthcare establishments promulgated together with Decision No. 5188/QD-BYT dated 14/12/2020 by the Minister of Health.
CARE OF SUSPECTED, ASYMPTOMATIC, MILD AND MODERATE COVID-19 CASES
1. Overview
- Suspected cases (may be regarded as an emergency condition) shall be examined, cared for monitored and isolated in a separate area in healthcare establishments, and have their samples collected properly for confirmatory testing.
- Mild cases (upper respiratory tract infection, mild pneumonia) shall be treated and cared for in isolation areas of normal departments.
- As there is no known effective cure, treatment mostly involves supportive care and symptom treatment.
- Treatments and care measures shall be individualized for each case.
- Severe conditions and complications must be monitored, detected and handled promptly.
2. Care
2.1. Assessment
- Physical condition, mental condition, skin, mucous membranes.
- Temperature, heart rate, blood pressure.
- Respiratory condition:
+ Respiratory rate, respiratory pattern, dyspnea level.
+ Oxygen saturation level (SpO2).
+ Symptoms: stuffy nose, cough, sputum, throat pain, chest pain and tightness.
- Other symptoms: digestion, urology, headache, muscle pain, etc.
2.2. Nursing interventions
2.2.1. Respiratory assurance
- Have the patient lie down with their head elevated; sitting and walking will help the patient's diaphragm function better and prevent sputum accumulation.
- Administer oxygen therapy (if necessary) according to indications.
- Administer clapping and vibration, instruct the patient on how to breathe slowly and deeply to prevent sputum accumulation.
- The patient needs to wear face masks and practice respiratory hygiene when coughing and spitting.
- Clean the nose and throat, can keep the nose moisturized with saline drops, gargle.
2.2.2. Physician order execution
- Carry out physician orders for infusion, injection and drug administration properly and promptly.
- Assist doctors with procedures where indicated.
- Conduct tests promptly and adequately according to indications.
- Execute other physician orders.
2.2.3. Nutrition assurance
- Evaluate the patient’s nutritional status on a daily basis.
- Provide meals and water at the patient’s bed throughout the isolation period.
- Encourage the patient to finish their meals and drink enough water, ensure fluid and electrolyte balances.
2.2.4. Health advice and education
- Immediately after the patient is admitted, inform the patient of the department’s rules and provide them with information sheets.
- Give encouragement and instructions about the disease to reassure the patient.
- Instruct the patient on diet, physical exercise, breathing exercise and therapeutic exercise.
- Instruct the patient on use of face masks, respiratory hygiene when coughing, hand hygiene and personal hygiene.
- Advise the patient on how to follow COVID-19 prevention guidelines at home after they complete their quarantine. The patient needs to check their temperature twice a day. If their temperature is higher than 38 degrees Celsius in two consecutive checks or there is any other abnormal sign, they must visit a healthcare establishment for examination immediately.
2.2.5. Complication monitoring and prevention
- Monitor respiratory rate, SpO2, heart rate, temperature and blood pressure at least twice a day and when necessary; promptly detect abnormal signs such as worsening dyspnea and respiratory failure to make suitable interventions.
- For patients with worsening pneumonia, notify the doctor and prepare equipment for endotracheal intubation/ tracheotomy and mechanical ventilation.
- Pay attention to patients aged 60 and older and patients with existing chronic diseases such as cardiovascular diseases, chronic pulmonary diseases, diabetes mellitus, cancer, etc.
2.3. Assessment
Good progress:
- The patient no longer has fever, has stable heart rate and blood pressure, does not develop respiratory failure, complications or nursing care accidents such as pneumonia, pressure ulcers, etc.
- The patient and their family understand about COVID-19, care methods and how to prevent COVID-19.
- Healthcare workers and the patient’s family are not infected with the disease.
No progress or worsening:
The patient’s general condition worsens. The patient develops severe respiratory failure, functional disorders, complications such as pressure ulcers, pneumonia, etc. or suffers from multiple sequelae or spreads COVID-19 to healthcare workers and their family.
CARE OF SEVERE AND CRITICAL COVID-19 CASES
Severe cases shall be treated in emergency rooms of departments or intensive care rooms in isolation areas. Critical cases shall be treated in special care rooms. Severe and critical cases require level 1 care in compliance with the following guidance:
I. COVID-19 cases with acute respiratory distress syndrome
1. Rules for care:
COVID-19 patients with acute respiratory distress syndrome (ARDS) shall be monitored and promptly handled to prevent fatality according to the “SAS” rule: Safe: safe for caregivers and patients; Accurate: avoid unreliable, unfamiliar or repetitive techniques; and Swift: not hasty or late.
Prevent transmission to healthcare workers during administration of oxygen therapy, high flow nasal cannula (HFNC), continuous positive airway pressure (CPAP), noninvasive ventilation (NIV), inspiratory positive airway pressure (IPAP) and expiratory positive airway pressure (EPAP).
2. Care
2.1. Assessment
- General condition: consciousness (wakefulness, contact, Glasgow coma scale), skin, mucous membranes, body temperature.
- Respiratory condition:
+ Respiratory rate, respiratory pattern, level of dyspnea, cyanosis, respiratory muscle contraction.
+ Oxygen saturation level (SpO2).
+ Symptoms: cough, sputum, throat pain, chest pain and tightness, etc.
- Other symptoms: digestion, urology, neurology (headache), muscle, bones, joints (muscle and joint pain, etc.).
2.2. Nursing interventions
2.2.1. Respiratory assurance:
- Take safety measures to minimize contact or droplet transmission. Place a medical mask on top of the nasal cannula when administering HFNC.
- Continuously monitor oxygen saturation before and during oxygen therapy administration. Some patients may develop rapid oxygen desaturation over time.
- The patient must wear a medical mask when they use the nasal cannula.
a. HFNC/ NIV:
- Monitor general condition: consciousness, skin, mucous membranes, face, vital signs, respiratory pattern, SpO2.
- Mask ventilation: the mask must fit the patient. Secure the mask properly to prevent pressure ulcers on the nasal bridge and oxygen leakage, which will decrease airway pressure and increase infection risk. Secure the mask behind the patient’s head above the ears and on the nape.
- Ensure airway is clear: instruct the patient on how to cough and spit out sputum or suction sputum for the patient (if necessary).
- May stop the therapy when the patient spits out sputum or eat and drink with their mouth.
b. Prone ventilation
- Closely monitor the patient’s respiratory state and consciousness. Prevent the tube from moving when the patient has endotracheal intubation.
- Keep the airway clear; prevent the oxygen tube or endotracheal tube from folding when the patient is in prone position and turned to another position.
- Properly handle the patient’s bodily fluids (saliva, nasal discharge, sputum, etc.) using a disinfectant containing chlorine (2500 mg/L).
2.2.2. Physician order execution
- Carry out physician orders for infusion, injection and drug administration properly, promptly and accurately.
- Perform paraclinical tests and functional tests according to doctor’s indications.
- Assist doctors with procedures where indicated. Irrelevant persons should not be present in a room where a procedure is being performed.
- Move the patient for X-ray, CT scanning, ultrasound, etc. in compliance with patient classification rules.
2.2.3. Complication monitoring and prevention
- Detect signs of respiratory failure and circulatory failure such as weak rapid pulse, hard to measure blood pressure, rapid breathing, retractions, blue lips, peripheral cyanosis, etc. early on.
- Detect aspiration in HFNC/ NIV and prone ventilation early on.
- Monitor and prevent pressure ulcers and venous thrombosis.
- Pay more attention to elderly patients and patients with existing chronic diseases such as cardiovascular diseases, chronic pulmonary diseases, diabetes mellitus, cancer, etc.
2.2.4. Nutrition
Ensure nutrition and improve the body’s condition. For severe - critical cases, follow nutrition recommendations of Vietnam National Association of Emergency, Intensive Care Medicine and Clinical Toxicology and indications of nutrition doctors.
2.2.5. Other monitoring and care
- Closely monitor respiratory rate, heart rate, blood pressure, temperature, SpO2; P/F and lactate level at least once every hour.
- Monitor urine output once every 3 hours; monitor daily fluid balance to ensure fluid and electrolyte balance.
- Reduce fever by cold compression. Administer antipyretics if when indicated.
- Clean and disinfect tools (stethoscopes, thermometers) before using them on a patient.
- Closely monitor short-term (<2 hours) NIV; if the patient has acute left ventricular failure, chronic obstructive pulmonary disease or immunodeficiency, administer endotracheal intubation as soon as possible if respiratory failure symptoms do not improve. Add a virus filter between the mask and valve for single-tube NIV. It is recommended to choose a suitable mask to reduce risk of transmission via air leakage.
- Monitor aspiration risk.
2.2.6. Pulmonary rehabilitation
- Instruct the patient on deep-slow breathing and chest-opening combined with shoulder-opening breathing techniques.
- Administer clapping and vibration as soon as possible.
- Provide physical rehabilitation early to help the lungs expand fully and prevent sputum accumulation.
- Turn the patient’s body regularly once every 2 - 3 hours, exercise the limbs to prevent muscle atrophy and joint stiffness.
2.3. Assessment
Good progress:
If the patient feels comfortable and breathes steadily without fatigue, and SpO2 is stable ≥ 95%, may reduce oxygen flow (with doctor’s indication).
No progress or worsening:
If the patient has worsening dyspnea, respiratory muscle contraction, blue lips, peripheral cyanosis and SpO2 ≤ 92%, notify the doctor immediately and prepare endotracheal intubation equipment as the patient may require ventilation.
II. Care of mechanically ventilated COVID-19 cases
1. Modes of mechanical ventilation in respiratory support
Mechanical ventilation is a process where medical gas and oxygen are mixed together in a predetermined ratio and pushed into the airway to reach the alveoli. When the lungs expand, pressure inside the alveoli also increases. When the signal for termination (usually for pressure or air flow) is emitted, the machine stops pushing air into the airway, which reduces airway pressure, followed by passive expiration with the air flow travels from the alveoli (high pressure) to the airway (lower pressure). Invasive ventilation is the most common mode of mechanical ventilation and is used to carry out a part or the whole natural respiration process by taking over respiration and gas exchange in patients with respiratory failure. Invasive ventilation provides positive pressure ventilation for the lungs via an endotracheal tube or tracheostomy tube while non-invasive ventilation provides ventilatory support via other tools, usually masks.
Modes of mechanical ventilation:
- Control ventilation, including continuous mandatory ventilation (CMV) and assist-control ventilation (A/C).
- Assisted ventilation, including synchronized intermittent mandatory ventilation (SIMV) and SIMV + PS (support for spontaneous breathing).
- Spontaneous ventilation, including PS and CPAP (no support for spontaneous breathing).
2. Rules for care of COVID-19 cases requiring invasive ventilation
- Use PPE according to regulations while giving care.
- Ensure that the whole ventilator circuit, especially joints on the tubes, has no leak. Act in a careful manner and avoid unnecessary disconnection when the endotracheal tube is inserted into a patient to prevent the virus from escaping outside (e.g., closed sputum suctioning equipment needs to be integrated with the circuit, if possible).
Clip the endotracheal tube when the circuit needs to be disconnected (such as for squeezing the ambu bag, switching to a mobile ventilator) and release it after the set is connected again. This is regarded as an aerosol generating procedure and should be performed in an isolated room if possible.
- Other precautions include use of circuits consisting of separate inspiratory and expiratory tubes with virus filters as well as heat and moisture exchangers (HME). Filters with HME should be placed between the expiratory portal and the endotracheal tube.
- It is of utmost importance to comply with standards for maintenance of endotracheal tube cuff pressure at 25 - 30 cm H2O to maintain a seal within the airway.
- All ventilators should have suitable filters, which shall be changed according to schedule. After each change, the ventilators shall be wiped clean.
3. Management of mechanically ventilated COVID-19 cases
- Mechanically ventilated COVID-19 cases should stay in negative pressure rooms.
- In case negative pressure rooms are unavailable, employ mixed air or natural ventilation and ensure that the minimum ventilation rate is 12 ACH.
- Locate entrance and exit as appropriate.
- Ensure that the rooms’ doors are always closed and have a warning sign with red background and yellow writing that reads “KHU VỰC CÁCH LY Y TẾ - KHÔNG NHIỆM VỤ MIỄN VÀO” (“MEDICAL ISOLATION AREA - UNAUTHORIZED ACCESS NOT ALLOWED”).
- Arrange for a hand washing area with water and soap or a hand sanitizer with at least 60% alcohol.
- Provide yellow containers with lids and foot pedals, lined with yellow bags used for infectious waste, and affixed with a “CHẤT THẢI CÓ NGUY CƠ CHỨA SARS- CoV-2” (“SARS-CoV-2 DANGERS”) label. All wastes from isolation areas shall be considered as infectious waste.
- Have plans to clean and disinfect surfaces at least twice a day and when necessary.
4. Care
4.1. For mechanically ventilated patients
4.1.1. Assessment
a. Patient’s general condition
- Vital signs: consciousness, heart rate, blood pressure, respiratory rate, temperature, SpO2.
- Skin and mucous membrane: pink or bluish.
- Breathing and chest movement.
- The patient’s cooperation with the ventilator, no ventilator resistance, sedation level.
- The patient’s response to the ventilator: lying still, pink skin and mucous membranes, no ventilator resistance, stable vital signs, satisfactory SPO2, normal blood gas.
- Sputum: quantity, color, properties.
- Stomach secretions: quantity, color, properties.
- Endotracheal tube: size, length, fixed location; cuff pressure.
- Additional fluids (if any): pleural fluid, pericardial fluid, urinary catheter, etc.
- Assessment of skin areas at risk of pressure ulcers: stomach catheter location, endotracheal tube location, heels, tailbone, pinna, elbows, etc.
b. Ventilators:
- Ventilator supply sources: power, oxygen, compressed air, etc.
- Ventilator settings: breathing mode, pressure, VTE, breathing rate, PIP, FiO2, etc.
- Warning levels.
- Humidity of circuit and filters.
c. Assessment of infection risk posed by mechanically ventilated patients:
- Risk of aerosol and droplet generation of patients.
- Necessary procedures.
- PPE.
- Compliance with infection prevention practices of healthcare workers.
4.1.2. Interventions:
Note: comply with regulations on use of PPE and cross-contamination control in care of COVID-19 cases.
a. Management of patients responding to tranquilizer and analgesics:
- Monitor vital signs and SpO2.
- Monitor levels of consciousness, sedation and pain; assess cooperation between the patient and the ventilator.
- Monitor and ensure dosage of tranquilizers in use.
- Monitor and detect complications such as prolonged coma, apnea, slow heart rate and hypotension early on.
b. Airway management:
- Monitor and evaluate the following ventilator settings:
+ VTE: exhaled tidal volume, especially for volume controlled ventilation, to detect air leak from the endotracheal tube and insufficient air input into the lungs.
+ VTE decrease:
* For volume controlled ventilation: VTE decrease means large air leak from the endotracheal tube, requiring a larger tube or a tube with a cuff.
* For pressure controlled ventilation: VTE decrease means the ventilator is unable to cover the amount of air leaking from the endotracheal tube or elasticity decreases and airway obstruction increases.
+ VTE increase: usually occurs when the patient’s condition improves; ventilator weaning or spontaneous breathing should be considered.
+ Peak inspiratory pressure (PIP):
* For volume controlled ventilation: PIP changes depending on lung elasticity and airway obstruction.
* PIP increase: occurs when lung elasticity decreases due to lung collapse, pneumothorax or pneumochysis or obstruction increases due to bronchospasm or obstructed endotracheal tube.
- Ventilator respiratory rate:
+ Ventilator’s respiratory rate being higher than the general setting means spontaneous breathing is involved.
+ Ventilator resistance: consider administration of respiratory inhibitors and tranquilizers.
+ Improvement of clinical condition and SpO2: start ventilator weaning.
- Ventilator warnings:
+ Air delivery system must be clean, closed and always placed lower than the endotracheal/ tracheostomy tube.
+ Prioritize locating HME filters at the inspiratory limb and before the expiratory limb of the ventilator. If humidification and heating systems are used, keep the water at permitted level, maintain the temperature at 30-350 degrees Celsius and check the presence of condensation. Place bacteria filters at the expiratory limb. The presence of condensation means excessive humidity, requiring lower temperature.
+ Sputum suctioning: use closed suctioning system, select a suctioning catheter of suitable size (catheter size = (inner diameter of endotracheal tube - 1) x 2), suctioning time ≤15 seconds.
Table 4. Suctioning pressure by age
|
Age |
Suctioning pressure |
|
Newborns |
50-80mmHg |
|
Children |
80-100mmHg |
|
Adults |
100-120mmHg |
c. Prevention of ventilator-associated pneumonia:
- Choose a suitable endotracheal tube. It is recommended to use a subglottic secretion drainage endotracheal tube and suction secretions every 2 hours.
- Use disposable circuits.
- Place HME filters at the inspiratory limb and before the expiratory limb of the ventilator.
- Elevate the patient’s head to 30 degrees (unless contraindicated).
- Monitor endotracheal tube cuff pressure every 4 hours and maintain it at 25 - 30 cmH2O.
- Take measures against hospital-acquired infection.
- Use sterile sputum suctioning technique and closed sputum suctioning system.
- Monitor the patient’s temperature and detect infection signs from sputum color, quantity and properties as well as complete blood count early on.
- Use new circuit for each patient; change the circuit only if it becomes soiled or damaged when the patient is put on the ventilator.
- Change heat and moisture exchangers when they are soiled or damaged or every 5-7 days.
- Regularly change the patient’s position.
- Clean the patient’s nose and mouth using chlorhexidine 0.2%; keep these areas clean and prevent secretion accumulation.
d. Monitoring and early detection of ventilator complications:
|
No. |
Complication type |
Sign |
Cause |
Handling |
|
1. |
Ventilator resistance |
Irritation, cyanosis, sweating, respiratory muscle contraction, rapid pulse, high blood pressure, low SpO2, etc. |
- Unsuitable breathing mode or settings - Spontaneous breathing due to insufficient tranquilizer - muscle relaxant - Endotracheal tube is obstructed, inserted too deeply or folded; or patient bites the tube - Pneumothorax |
- Inform doctor - Check circuit and ventilator - Squeeze ambu bag with Fi02 at 100% - Suction sputum from endotracheal tube, nose and mouth |
|
2. |
Endotracheal tube slipping out |
- Cyanosis, no breathing sound from ventilator - Low exhaled volume warning from ventilator |
- Improper tube securing - Patient thrashing |
- Do bag mask ventilation with filter between mask and bag - Insert new endotracheal tube |
|
3. |
Obstructed endotracheal tube |
- Irritation, sweating, low SpO2 - High airway pressure warning from ventilator |
- Sputum or inserted too deeply |
- Suction sputum - Adjust tube - Insert new tube |
|
4. |
Pneumothorax |
Sudden cyanosis, irritation, unequal chest expansion, decreased or no breath sounds on one side, possible subcutaneous emphysema |
- Too high pressure or tidal volume setting - Improper respiratory inhibition - Ventilator resistance |
- Chest X-ray, emergency chest drain - Adjust settings as suitable |
|
5. |
Lung collapse |
Decreased or no breath sounds on one side |
Endotracheal tube is inserted too deeply into one lung side Sputum - Not changing patient's position regularly |
- Clapping and vibration - Suction sputum -Postural drainage - Change patient’s position every 2-3 hours - Elevate head |
e. Prevention of reflux and aspiration:
- Elevate the patient’s head to 30 - 45 degrees (if not contraindicated).
- Check and evaluate residue stomach secretions every 4 - 6 hours, stomach, feces and gastrointestinal hemorrhage.
Use feeding tubes made from soft materials (silicon; polyurethane) for prolonged period of time.
- Monitor digestion in the intestines.
g. Management of urinary tract and other types of drainage:
Monitor and prevent urinary and reproductive tract infections and correctly measure daily urine output depending on whether the patient uses diapers, incontinence pads or a urinary catheter.
For other cannulae: monitor quantity, colors, etc. of secretions.
h. Management of fluid input - output:
Monitor fluid balance to ensure input - output balance.
i. Prevention of pressure ulcers:
- Add padding under skin areas placed under pressure; administer Sanyrene to reddened skin areas.
- Use a pressure-relief mattress with a thickness of at least 20 cm or air mattress.
- Change the patient’s position every 3 hours (supine, right lateral, left lateral) if not contraindicated.
- Evaluate the patient’s skin condition regularly, manage secretions to ensure that the skin is always dry and clean.
k. Prevention of deep vein thrombosis:
- Change the patient’s position and do passive exercise to prevent circulatory stagnation as soon as possible.
- Check the vascular system to detect thrombosis, arterial thrombosis or venous thrombosis, and inform the doctor for timely handling.
l. Nutrition for mechanically ventilated patients:
- Ensure nutrition and improve the body’s condition. For severe - critical cases, follow nutrition recommendations of Vietnam National Association of Emergency, Intensive Care Medicine and Clinical Toxicology and indications of nutrition doctors.
- Combine enteral and parenteral nutrition.
4.2. Care of patients weaning from ventilators
4.2.1. Ventilator weaning conditions:
|
Ventilator setting |
Patient’s condition |
|
- Gradually reduce the following ventilator settings in order of priority before weaning: - Gradually reduce PIP to < 35cm H2O. - Gradually reduce FiO2 to < 60%. - Gradually reduce I-time to < 50%. - Gradually reduce PEEP to < 8cm H2O. - Gradually reduce FiO2 to < 40%. - Gradually reduce PEEP, PIP, I-time and respiratory rate. - Consider switching to breathing support if currently on control ventilation to start weaning from ventilator
|
- Cause(s) of respiratory failure has/ have been treated. - Improved consciousness or no more convulsions. - Stable spontaneous breathing, sufficiently strong coughing reflex. - Good blood oxygen level: SpO2 ≥ 95% with FiO2 ≤ 40%. - PEEP ≤ 5 cm H2O, Pi ≤ 18 cmH2O. - Blood gas: PO2≥80mmHg with FiO2≤ 40%; PCO2 = 35 - 40mmHg. PaO2/FiO2≥ 300 - Stable hemodynamics; no or low-dose administration of vasoactive drugs. - Normal pulse and blood pressure. - No fever or mild fever (temperature < 38oC). - Chest X-ray shows improvement with little or no infection. - Good nutritional status, no anemia (Hct ≥ 30%), good response to enteral tube feeding. |
4.2.2. Monitoring during ventilator weaning:
When the patient is weaning from the ventilator, nurses must stay with them to monitor and encourage them. If the patient shows sign of weaning failure, put the patient back on the ventilator immediately.
Signs of failure with spontaneous breathing:
- Sweating, irritation.
- Increased respiratory rate (≥ 20% of normal rate for age).
- Increased heart rate.
- Increased or decreased blood pressure.
- Retractions.
- SpO2 < 92%.
- Worsening blood gas.
4.2.3. Notes for ventilator weaning:
- Stop administering all muscle relaxants and tranquilizers for at least 2 hours.
- Stop enteral tube feeding for at least 2 hours.
- Carry out ventilator weaning in the morning when there are sufficient staff and experienced doctors.
- If the patient shows signs of weaning failure, put them back on the ventilator.
4.3. Assessment
Good progress:
- The patient feels comfortable and can breathe naturally without fatigue and with the endotracheal tube removed; SpO2 ≥ 95%.
No progress or worsening:
- Increased dyspnea, respiratory muscle contraction, continuous ventilator resistance, increase of tranquilizer and vasoactive drug dosages.
- No improvement in oxidative stress.
- No improvement in blood oxygen when put on ventilator; nurse shall prepare ECMO equipment.
III. COVID-19 cases requiring emergency hemofiltration
1. Overview
Emergency hemofiltration, also known as renal replacement therapy, is a treatment that aims to remove wastes and soluble substances using semi-permeable membranes, which is similar to the filtration process in the kidneys.
Hemofiltration in COVID-19 patients aims to remove toxins and perform liver and kidney functions.
Extracorporeal hemofiltration techniques include intermittent hemofiltration, continuous hemofiltration, plasma replacement, hemoperfusion, etc.
Purposes of emergency hemofiltration:
- Replace kidney functions.
- Ensure water, electrolyte and acid - base balances.
- Reduce toxic substances such as urea, creatinine, etc. in blood.
Rules for safety in care: take standard precautions in combination with precautions against contact and droplet transmission in patient care.
2. Complications
* Catheter-related complications:
Immediate complications: inserting the needle into an artery, blown veins, hematoma, retroperitoneal bleeding, hemothorax, pneumothorax and gas embolism.
Late complications: thrombus, infections, arteriovenous fistula.
* Treatment-related internal complications:
- Hemodynamics: hypotension, arrhythmia.
- Bleeding.
- Electrolyte or acid - base disorder.
- Dialysis disequilibrium syndrome.
* Technical complications:
- Gas embolism:
- Blood loss, thalassemia.
- Hypothermia.
- Coagulation in filter membranes and tubes.
- Tube and catheter slipping or twisting.
- Allergy to filter membranes.
3. Care
3.1. Assessment
- Evaluate consciousness level, physical condition and mental condition of the patient.
- Vital signs, respiratory condition.
- Vessels used for filtration.
- Daily water input - output, weight, edema.
- Skin and mucous membrane conditions, signs of anemia, hemorrhage, etc.
- Diet, intravenous fluids and drugs administered daily.
- Risk of infection via direct contact with the patient, environmental surfaces, filtration equipment, wastes, including post-filtration waste fluids, and droplets from close contact (< 2 meters).
3.2. Nursing interventions
3.2.1. Before hemofiltration:
- Inform and give explanation to the patient.
- Evaluate consciousness level, heart rate, blood pressure, respiratory rate, temperature, SpO2 of the patient.
- Perform biochemical tests, coagulation factor tests and other tests according to physician orders.
- Clean the catheter insertion site.
3.2.2. During hemofiltration:
- Replace filtration fluids using the correct technique.
- Administer medications as per physician orders, check Heparin dosage.
- Check catheter location (obstructed or slipping), filter membranes and air traps (coagulation in filter membranes and air chamber, membrane breaking).
- Perform personal hygiene for the patient and execute other physician orders for care.
3.2.3. After hemofiltration:
- Check heart rate, temperature respiratory rate, blood pressure, consciousness level and urine after hemofiltration is completed.
- Record the patient’s developments during the hemofiltration process.
- Take care of the filtration catheter: prevent clotting using Heparin and change bandages. If there are signs of infection (red swelling, pus), notify the doctor, remove the catheter, and obtain blood culture from catheter tip.
- Clean and disinfect bed surface and equipment using disinfectants.
- Solid waste shall be handled as highly infectious waste and put in a yellow nylon bag labeled “chất thải có nguy cơ chứa Sars-Cov-2” (“Sars-Cov-2 dangers") in the isolation room, which shall be put inside another bag outside of the isolation room, before it may be moved to the waste storage facility of the healthcare establishment.
- Waste fluids from filtration shall be processed in the common medical wastewater treatment system of the healthcare establishment. If this system does not meet environmental standards, waste fluids must be disinfected using a chemical solution containing 1,0% activated chlorine before they may be discharged outside. Filtration fluid containers shall be handled immediately after each filtration and must not be shared between patients.
3.2.4. Nutrition assurance:
- Evaluate the patient’s nutritional status.
- Provide nutrition according to physician orders.
- Encourage the patient to finish their indicated meals.
- Monitor intake, water input - output and weight.
3.2.5. Health advice and education:
- Give encouragement and explanation for the patient to understand the necessity of hemofiltration and have trust in their treatment.
- Give instructions on drug use, diet and water intake required for the patient's condition.
- Give instructions on how to monitor and care for the filtration catheter site to prevent complications.
3.2.6. Complication monitoring and prevention:
- Monitor results of biochemical tests and coagulation factor tests before and after hemofiltration.
- Monitor consciousness level, heart rate, blood pressure, respiratory rate, temperature, SpO2, and water input - output of the patient every 2 hours during and after hemofiltration until the patient's condition stabilizes.
- Monitor to detect allergic signs such as rashes, dyspnea and anaphylactic shock early on.
- Monitor settings and warnings of the hemofiltration machine, filter system and air trap.
- Monitor signs of hemorrhage such as skin and mucous membrane conditions and bleeding at catheter insertion site.
- Monitor signs of blood infection and infection at catheter insertion site.
3.3. Assessment
Good progress:
- Respiratory failure, hemodynamic disorders, electrolyte disorders and renal dysfunction gradually improve; edema is reduced; there is no complication or accident related to hemofiltration.
- Healthcare workers, other patients and the patient’s family are not infected with the disease.
No progress or worsening:
- Respiratory failure, hemodynamic disorders, electrolyte disorders and/or renal dysfunction do/does not improve or worsen/s; edema remains unchanged or increases; there are decreased or no urine output and complications or accidents related to hemofiltration.
- Healthcare workers, other patients and the patient’s family are not infected with the disease.
IV. COVID-19 patients having sepsis and septic shock
1. Overview
Approximately 5% of COVID-19 patients require intensive care with acute respiratory manifestations (rapid breathing, dyspnea, cyanosis, etc.), ARDS, septic shock and organ dysfunction, including kidney injury and heart muscle injury, leading to death. These cases need to be monitored and handled promptly.
There is risk of infection via:
- Droplets
- Contact
- The air
Rules for safety in care: take standard precautions in combination with precautions against contact, droplet and airborne transmission in patient care.
2. Care
2.1. Assessment
2.1.1. Questioning: promptly evaluate the patient: consciousness level, vital signs. Find severe signs of shock, preliminary shock orientations and cause.
Quickly discuss with the doctor to grasp the patient’s current condition and development trend thereof.
Give an explanation on the situation to the patient if they are conscious or to the patient’s family if the patient is in coma.
2.1.2. Physical examination: determine sepsis level and clinical manifestations
Sepsis: somnolence, stupor, coma, dyspnea? or rapid breathing, low oxygen saturation level; fast pulse, weak pulse, cold limbs, or low blood pressure, livedo reticularis; decreased or no urine output; test results indicating coagulation disorders, thrombocytopenia, acidosis, increased lactate level, increased bilirubin level, etc.
Septic shock: low blood pressure? narrow blood pressure? or fluctuating blood pressure, unmeasureable blood pressure in serious cases; temperature at 36 or <=35 degrees; rapid breathing; dyspnea, cyanosis? respiratory failure? Manifestations of circulatory failure and water and electrolyte disorders? Rapid, weak and hard to measure pulse, livedo reticularis, hypothermia, cold limbs? decreased (< 30ml/hour) or no (< <10ml/hour) urine output; at late stage: arrhythmia, possible cardiac arrest, low and unmeasureable blood pressure. Consciousness: stupor, exhaustion; panic and irritation; and coma in severe cases.
2.1.3. Infection risk:
There is risk of infection from direct contact with the patient, environmental surfaces, medical and care equipment (ventilators, monitors, pulse oximeters, etc.), wastes; droplets from close contact (< 2 meters); and the air when performing aerosol generating procedures on the patient (open sputum suctioning, NIV, etc.).
2.2. Nursing interventions
2.2.1. Airway control and maintenance to ensure ventilation:
- Lower the patient’s head if they have low blood pressure and turn the face to one side to prevent reflux. Give the patient oxygen at a flow rate of 4-6 liters/minute, or oxygen mask according to indications.
- Use a Mayo tube to prevent tongue retraction; suction sputum and saliva in the mouth and throat.
- Squeeze Ambu bag if the patient stops breathing or breathes weakly.
- Prepare equipment and additional ventilators to assist the doctor with intubation and ventilation where indicated.
- Closely monitor respiratory rate, respiratory pattern and SpO2 every 15-30 minutes when the patient has respiratory failure.
- Monitor the patient if they are mechanically ventilated. Monitor patient’s response to the ventilator and the ventilator’s operation.
- Use closed sputum suctioning system if the patient is mechanically ventilated (to prevent airborne transmission) and observe sputum quantity, color and properties.
2.2.2. Blood loss replacement:
- Immediately insert a peripheral venous catheter; promptly administer fluids, blood or vasoactive drugs according to indications.
- Prepare equipment and assist the doctor with inserting a central venous catheter.
- Prepare transfusion equipment, electric syringe pumps, intravenous fluids and vasoactive drugs according to physician orders.
- Set up monitors; keep the patient warm in case they have hypothermia.
- Monitor the patient’s hemodynamics such as pulse, blood pressure and temperature every 15 - 30 minutes; monitor capillary refill time.
- Monitor urine output every hour. Measure central venous pressure.
- Immediately notify the doctor of abnormal parameters to adjust vasoactive drugs, transfusion rate, etc.
2.2.3. Monitor water and electrolyte conditions:
- Evaluate overhydration signs such as chemosis, anasarca, acute pneumochysis and central venous pressure >15 cm H2O.
- Or dehydration signs such as dry and wrinkled skin, dry lips and mouth, dry tongue and CVP<2 cm H2O.
- Collect blood samples for electrolyte panel; perform an arterial blood gas test.
- Handle acid - base imbalance according to indications.
- Monitor the patient’s weight, fluid input (fluid transfusions, blood transfusions, water, food) - output (urine, vomit, etc.) balance, central venous pressure and electrolyte panel levels.
2.2.4. Adequate and timely execution of medication and testing orders:
- Prevent shock: transfuse approximately 500 ml fluids or colloids within the first 30 minutes - 1 hour to replace blood loss according to indications. Make a clinical assessment and adjustment. Administer vasoactive drugs as indicated; use electric syringe pumps and transfusion machines to ensure transfusion rate of dopamine, noradrenaline, etc. Transfuse blood and blood preparations in compliance with regulations on blood transfusion safety.
- Administer antibiotics: collect samples to identify the bacterium/a causing superinfection before administering antibiotics as indicated.
- Collect samples for basic tests, blood glucose control, chest X-ray, abdominal ultrasound and heart ultrasound.
Collect respiratory samples (throat and nose swabs, throat and mouth swabs, sputum, bronchial fluids, bronchial wash) to test for SARS-CoV-2.
2.2.5. Assurance of patient’s nutrition and personal hygiene:
- Nutrition: provide the patient with a protein-rich fluid-based diet with sufficient calories; use enteral tube feeding or parenteral feeding for patients in coma or unable to eat.
- Personal hygiene: assist the patient with dental hygiene 2-3 times/day or after a meal.
Wash the patient’s eyes and give them eye drops on a daily basis. For comatose patients, cover their eyes with sterile gauze pads to prevent dry eyes.
Clean the patient’s body, genitalia and anus using warm water on a daily basis, ensure that the patient is always cleaned and keep the patient warm in cold season (using heaters instead of air-conditioners). Change the sheets and the patient’s clothing on a daily basis (turn the patient left and right gently, do not raise their head, etc.). Lay the patient on a waterbed or pressure-relief mattress to prevent pressure ulcers, and change the patient's position every 2 - 3 hours. Take measures to control bowel and/or urinary incontinence.
- Clap and vibrate the patient’s chest (after shock stage); exercise the patient’s limbs gently.
2.2.6. Health advice and education for patients:
If the patient is not comatose, regularly give them encouragement. Always be ready to carry out the patient’s requests to help them feel rest assured and cooperate in the treatment process.
Explain the patient’s condition, development trend thereof and possible unfavorable scenarios to the patient's family.
Explain the infection risk to the patient’s family for prevention (do not let the patient’s family, who have no professional knowledge about infection, take care of them).
2.2.7. Complication monitoring and prevention:
- Respiration: monitor respiratory condition (SpO2, blood gas, etc.), ventilator response, etc.
- Renal failure: monitor urine output every hour, urea, creatinine, electrolyte panel, etc. Prepare equipment for continuous renal replacement therapy and assist the doctor with hemofiltration.
- Cardiovascular complications: set up monitors for heart rate, blood pressure and response to vasoactive drugs. Monitor arterial blood pressure continuously. Monitor endocarditis, pericarditis and arrhythmia.
- Hemorrhage and coagulation disorders:
+ Hemorrhage: cyanosis, necrosis.
+ Gastrointestinal hemorrhage (haematemesis, bloody stool).
+ Monitor results of coagulation factor tests: prothrombin, D- dimer, Hb, erythrocytes, platelets, etc.; monitor capillary refill time if it is longer than 2 seconds.
2.2.8. Assessment:
The patient is well taken care of when:
- The patient is conscious and comfortable with temperature remaining stable at 36,5 - 37 degrees.
- Normal blood pressure, capillary refill time is less than 2 seconds.
- Urine output is more than 100ml/hour.
- Respiration: the patient breathes easily, SpO2 > 94%.
V. COVID-19 cases requiring ECMO
1. Overview
Extracorporeal membrane oxygenation (ECMO) is a resuscitation technique of providing respiratory and/or cardiac support to persons sustaining severe lung injuries and/or reversible heart injuries or persons not responding to common treatments. ECMO works by using an external pump (extracorporeal centrifugal pump or roller pump) to deliver the patient’s venous blood (not oxygenated) pass an artificial oxygenator, allowing oxygenation of the blood and removal of carbon dioxide, and then return the oxygenated blood to the patient’s circulatory system.
There are 2 main types of ECMO:
- VA - ECMO, which supports hemodynamics maintenance and gas exchange.
- VV - ECMO, which supports the lungs.
Purposes of ECMO:
- Provide sufficient oxygen for the patient.
- While ECMO does not treat the patient’s heart or lungs, it helps the patient overcome the critical stage and supports their treatment.
- Reduce heart medications.
- Reduce ventilator use to decrease risk of ventilator-related lung injury.
ECMO complications:
- Bleeding due to continuous use of anticoagulants and thrombocytopenia.
- Pulmonary vascular obstructive disease caused by a blood clot formed in the ECMO machine.
- Coagulation disorders resulting in blood clotting.
- Catheter-related complications.
- Infections.
- Stroke.
- ECMO technical issues.
There is risk of infection via:
- Droplets
- Contact
Rules for safety in care: take standard precautions in combination with precautions against contact and droplet transmission in patient care.
2. Care of COVID-19 cases requiring ECMO
2.1. Assessment
- General condition: consciousness, skin, mucous membranes, body temperature?
- Respiratory condition:
+ Respiratory rate and pattern.
+ Oxygen saturation level (SpO2).
+ Cough, sputum.
- Circulatory condition: heart rate, blood pressure, temperature, inotropic drugs, peripheral perfusion (foot dorsum, extremities).
- Other symptoms such as urology (urine output and color), digestion (stomach condition, feces, stomach fluids) and skin (areas affected by pressure ulcers).
- Catheter/cannula tip, ECMO machine.
- Risk of infection via direct contact with the patient, environmental surfaces, ECMO machine, ventilators, wastes, and droplets from close contact (< 2 meters).
2.2. Nursing interventions
2.2.1. Care of venous catheters of patients requiring ECMO
- Observe and evaluation the catheter’s fixed location (whether it has slipped in or out), inflammation (reddened, swollen, etc.).
- Prepare emergency equipment (tube clamps, crank handles, oxygen supply).
- Prevent cannula slipping.
- Change the bandages around the cannula carefully in a sterile manner, control and observe the cannula's tip (may be bleeding).
- Change bandages and place paddings to prevent pressure ulcers induced by medical devices.
- Monitor limb temperature, color and movements.
- Monitor heart rate.
- Monitor tubing and oxygenators.
2.2.2. Respiratory assurance:
- Monitor respiratory rate and SpO2.
- Monitor respiratory muscles and nose movements; check airway obstruction every 1-2 hours.
- Check skin color (this symptom might not be reliable in patients with hypothermia).
- Check arterial blood gas level values every two hours (blood gas before and after the oxygenator, patient’s blood gas).
- Monitor response to tranquilizers and anesthetics administered to the respiratory system.
- Monitor disorders such as anxiety, aggression and insomnia.
- Monitor the patient’s response to mechanical ventilation.
- Use closed sputum suctioning system if the patient is mechanically ventilated (to prevent airborne transmission) and observe sputum quantity, color and properties.
- Monitor arterial and peripheral oxygen saturation (SpO2).
- Check tube cuff pressure.
- Provide dental care for the patient on a daily basis to prevent bleeding.
2.2.3. Monitoring and prevention of complications and infection risks:
- Monitor ECMO operation (check presence of air, blood clots, etc.), including perfusion support, control of hemodynamic values and other important values, monitor respiratory readings and record into the monitoring sheet.
- Hemorrhage:
+ Check bandages (cannula tip) and blood buildup around the cannula.
+ Monitor and notify coagulation test results promptly.
+ Monitor bleeding via urine, feces, vomit, nosebleeds, epilepsy, diarrhea or pathological bruising on the skin.
+ Monitor brain hemorrhage (consciousness level, vital signs, pupils, muscle weakness or paralysis, etc.).
- Infections.
+ Monitor signs such as reddened or hot skin and elevated temperature.
+ Monitor blood test results (leukocyte, protein level, albumin level, blood cultures, CRP, etc.).
+ Evaluate quantity, color and properties of respiratory tract secretions.
+ Comply with sterile procedure/ surgery requirements.
- Pressure ulcers:
+ Assess risk of pressure ulcers and take preventive measures (use waterbeds or air mattresses).
+ Change the patient’s position every 2 hours, pay attention to ECMO tubing.
+ Take care of the patient’s skin properly, regularly moisturize the skin, and keep the skin clean after urination or defecation.
- Minimize infection risk:
+ Clean and disinfect bed surface and equipment using disinfectants authorized by the Ministry of Health.
+ Solid waste shall be handled as highly infectious waste and put in a yellow nylon bag labelled “chất thải có nguy cơ chứa -SARS-CoV-2” (“COVID-19 dangers") in the isolation room, which shall be put inside another bag outside of the isolation room, before it may be moved to the waste storage facility of the healthcare establishment.
2.2.4. Nutrition assurance:
- Administer an enteral feeding tube, always check the tube’s location, record feeding volume and leftover (if any).
- Provide parenteral nutrition with suitable quantity and components to ensure sufficient daily dietary intake.
2.2.5. Mental care, personal hygiene and health education:
- Give explanation and encouragement to the patient. Provide comprehensive care, including personal hygiene, dental care, prevention of hospital-acquired pneumonia, skin moisturization, daily bed linen change and prevention of pressure ulcers using suitable mattresses.
- Notify and explain to the patient before providing care services.
- Communicate non-verbally to explain to the patient why they could not talk, use papers, pens, etc. to explain care procedures.
2.3. Assessment:
Good progress:
- Stable vital functions.
- The patient has improved lung functions and is weaned from the ventilator; ECMO weaning (gradually decrease ECMO blood flow, gradually decrease ECMO air flow to 0, etc.) and ECMO cannula removal are being considered.
- The patient has improved heart functions, is weaned from VA ECMO and has the ECMO cannula removed.
No progress or worsening:
The patient’s general condition worsens, severe respiratory failure occurs, heart and lung functions do not improve, ECMO is ineffective.
CARE AND MANAGEMENT OF PREGNANT WOMEN SUSPECTED OR CONFIRMED TO HAVE COVID-19
1. Overview
During pregnancy, women experience physiological changes in their immune, respiratory and circulatory systems, thus, they have higher chance of severe illness and mortality in respiratory tract infection. SARS-CoV and MERS-CoV can cause serious pregnancy complications such as respiratory failure requiring endotracheal intubation or intensive care and renal failure. COVID-19 mortality rate among pregnant women are 25%. However, there is no study indicating that pregnant women face the risk of more severe COVID-19 infection or pneumonia.
Viral pneumonia increases the risk of premature birth, fetal growth retardation (FGR), low-weight birth, APGAR score at 5 minutes being under 7 and neonatal death compared to the non-pneumonia group (n = 7310).
Fever is a common COVID-19 symptom. A study of 80.321 pregnant women showed that the rate of fever in early pregnancy was 10% and the rate of fetal malformations was 3,7% while 8.321 cases were reported having fever above 38 degrees Celsius for 1 - 3 days in early pregnancy with no change in fetal malformation rate (odd ratio [OR] = 0,99) (KTC 95%, 0,88 - 1,12).
According to FIGO 2020, chest CT-scanning has high sensitivity for assessment of the condition of pregnant women with COVID‐19. However, it is necessary to explain the technique to pregnant women and their families, obtain their consent and cover the women’s abdomen during the scanning process. FGR, microcephaly, and intellectual disability are the most common adverse effects from high‐dose (>610 mGy) radiation exposure. When a pregnant woman undergoes a single chest X‐ray examination, the radiation dose to the fetus is 0,0005–0,01 mGy, which is negligible, while the radiation dose to the fetus is 0,01-0,66 mGy from a single chest CT or CT pulmonary angiogram.
2. Care of pregnant women suspected or confirmed to have COVID-19
2.1. Outpatient care
Obstetric facilities should employ telemedicine as much as practicable to provide prenatal care (consultancy) in compliance with recommended social distancing measures.
Recommended prenatal care schedule for low-risk pregnancy (to reduce exposure and workload in case of workforce shortage)
|
No. |
Gestational age |
Physical examination |
Ultrasound |
Task |
|
1 |
# 12 weeks |
In person |
Nuchal translucency |
Obtain past medical history First-trimester screening tests Provide health education: nutrition, precautions against droplet and contact transmission, and COVID-19 symptoms Provide antenatal care schedule |
|
2 |
# 16 weeks |
Online examination |
|
|
|
3 |
# 20 weeks |
In person |
Morphology |
Tripple test, amniocentesis (if applicable) Provide instructions on blood pressure monitoring at home |
|
4 |
# 24 weeks |
Online examination |
|
Monitor blood pressure at home |
|
5 |
# 28 weeks |
In person |
|
Regular checkup Oral glucose challenge test Inject Anti-D if the mother has negative rehsus blood type Provide instructions on fetal movement monitoring |
|
6 |
30 weeks |
Online examination |
|
Monitor blood pressure at home |
|
7 |
32 weeks |
In person |
Fetal development assessment |
Regular checkup |
|
8 |
34 weeks |
Online examination |
|
Monitor blood pressure at home Monitor fetal movements |
|
9 |
36 weeks |
In person |
|
Regular checkup GBS screening |
|
10 |
37-40 weeks |
In person |
|
Regular checkup Formulate delivery plan |
2.2 Inpatient care
2.2.1 Hospitalization: undergo screening at the gate of the healthcare establishment
Flowchart of intrapartum and postpartum maternal management
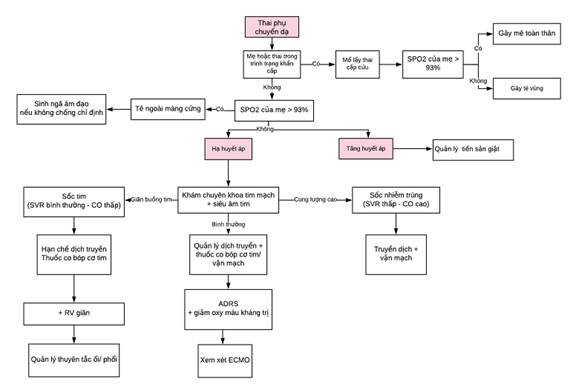
2.2.2 Monitoring of vaginal labor and delivery: in specialized negative pressure room
In case of miscarriage, the placenta/ fetus shall be handled as infectious tissues and may be tested for SARS-CoV-2 via qRT-PCR if necessary. Adhere to the national guidelines for reproductive healthcare services promulgated together with Decision No. 4128/QD-BYT dated 29/7/2016 by the Minister of Health.
|
No. |
Monitored item |
Early labor |
Active labor |
Nursing interventions |
Evaluation |
|
1 |
Vital signs: heart rate, blood pressure, temperature, respiratory rate, oxygen saturation Respiratory infection symptoms Cough, fever, diarrhea, dyspnea |
Regular: every 4 hours Progressing illness: every hour |
Administer drugs in compliance with treatment requirements Progressive illness: monitor using monitoring equipment Administer oxygen therapy Lower body temperature by wiping Record water input - output. Give instructions on mask use and hand hygiene |
Oxygen saturation level ranges between 92 - 95%. There is no fever and no dehydration signs. |
|
|
2 |
Fetal heart rate |
Every hour |
Monitor fetal heart rate and contractions continuously |
Give instructions on positions and breathing techniques for each labor phase Monitor using monitoring equipment |
Fetal heart rate is stable and ranges between 120 – 160 bpm on average. Check fetal heart rate before and after ROM/ amniotomy. |
|
3 |
Contractions |
Every hour |
Monitor fetal heart rate and contractions continuously |
Labor progresses as appropriate to each labor phase Early labor lasts for 8 hours. Active labor lasts for a maximum of 7 hours. |
|
|
4 |
Amniotic sac condition |
Every 4 hours |
Every 2 hours |
Perform physical examination at the appropriate time Inform labor situation to the mother |
|
|
5 |
Lightening degree |
Every hour |
Every 30 minutes |
||
|
6 |
Cervical dilation rate |
Every 4 hours |
Every 2 hours |
||
|
7 |
Epidural analgesia: pain, leg movements Dressing over epidural insertion site Catheters and electric syringe pumps |
|
Maintain dosage in compliance with treatment requirements Check dressing Evaluate level of loss of pain sensation and leg movements Prevent infection at catheter joinings |
The mother’s pain is reduced; epidural analgesia system is not obstructed. Joinings are protected by gauze pads. |
|
2.2.3 Cesarean delivery:
It is recommended to perform Cesarean sections in negative pressure operating rooms to protect healthcare workers and use appropriate PPE when performing aerosol generating procedures such as endotracheal intubation.
2.2.4 Postpartum care:
If both mother and baby are healthy, place the baby in the same room with the mother in a bassinet that is 2 meters away from the mother or has a physical divider such as a curtain. No viral ADN has been found in breast milk so far. Healthcare workers shall provide the mother with assistance and instructions for hand hygiene, use of 3-layer face masks upon close contact and breastfeeding.
The mother may experience anxiety and depression. Healthcare workers need to pay attention to her mental health and promptly assess her sleep pattern as well as causes of anxiety or depression or even suicide.
3. Care of babies born to mothers suspected or confirmed to have COVID-19
Immediately after birth, healthcare workers wearing suitable PPE shall promptly evaluate whether the baby requires resuscitation to move the baby away from other workers and place it in an incubator for breathing support. Babies born to mothers confirmed to have COVID-19 are not required to be admitted to the pediatric department. Such admittance shall be considered based on other criteria. Regularly monitor and assess the baby for infection signs.
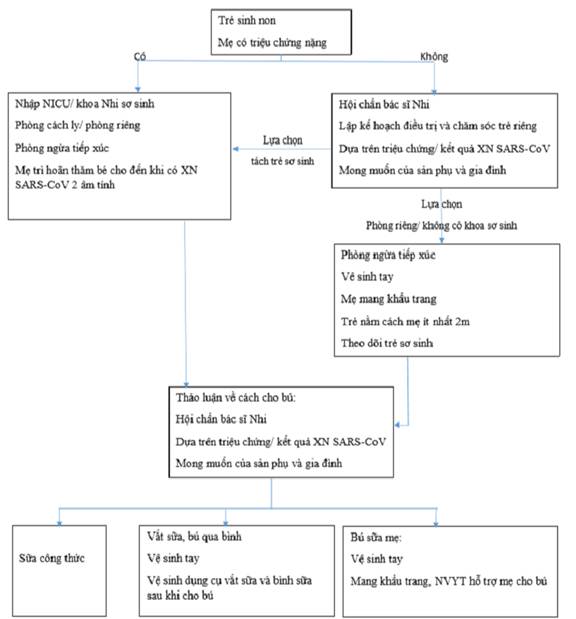
4. Nutrition care
No food can prevent or cure COVID-19 during pregnancy. Some food that is rich in antioxidants (vitamins C, E and A), protein, iron, zinc, selenium, omega 3 and omega 6 may strengthen the immune system. Healthcare workers shall give advice according to the national guidelines on nutrition for pregnant women and breastfeeding mothers (Decision No. 776/QD-BYT dated 08/3/2017 by the Minister of Health). Ensure food safety during purchase; store and process food at recommended temperatures.
- Provide at least three main meals as well as one nutritious snack for the first trimester and two nutritious snacks for the second and third trimesters.
- Each meal must include food that provides energy and builds the body and healthy food.
- Continue to supplement micronutrients (iron, folic acid and calcium) daily.
- Consult the nutrition and obstetric departments if the mother gains too much or too little weight during pregnancy or has anemia.
- Drink enough water (8-10 glasses of drinking water).
- Pregnant women should rest for 2 hours during the day and sleep for 8 hours at night.
- Do light exercise for at least 20-25 minutes every day.
Follow guidelines for hand hygiene, use of face masks, keeping safe distance of at least 1 meter, not touching the face when going shopping to minimize infection risk, and avoiding crowded places.
5. Health advice and education
There is no evidence that a baby may be infected with SARS-CoV-2 from its mother or during childbirth if its mother has COVID-19.
Pregnant women who have COVID-19 are not required to have a C-section unless otherwise indicated.
Unless the mother requires intensive care, it is recommended to let the baby have skin-to-skin contact and breast milk early in compliance with requirements for hand hygiene, surface hygiene, use of face masks upon any contact with the baby and placing the baby 2 meters away from the mother. It is not necessary to wear a face shield for the baby as it increases the risk of suffocation and the screen is not secured.
Provide instructions on postpartum care of the mother (including care during 6 weeks after birth, breastfeeding and contraception) and baby (including health, nutrition and jaundice monitoring and vaccination) according to the national guidelines for reproductive healthcare services promulgated together with Decision No. 4128/QD-BYT dated 29/7/2016 by the Minister of Health.
6. Progress and complication monitoring
All pregnant women should be monitored for development of symptoms and signs of COVID-19 (which are similar to those in nonpregnant individuals), particularly if they have had close contact with a confirmed or suspected case. Common symptoms include fever, cough, dyspnea, loss of taste, muscle pain, diarrhea and throat pain. However, in a systematic review involving 77 studies of 11.432 pregnant women, 7% tested positive for COVID-19 and 3/4 of them are asymptomatic
CARE OF CHILDREN SUSPECTED OR CONFIRMED TO HAVE COVID-19
1. Overview
Children make up 1% of total global COVID-19 cases. Clinical symptoms from incubation to recovery in children are similar to those found in adults. However, children have mostly milder clinical manifestations or no symptoms. Common signs in children include fever, cough or pneumonia manifestations. Children are less likely to have severe and critical cases than adults.
There is risk of infection via:
- Droplets
- Contact
- The air
Rules for safety in care: take standard precautions in combination with precautions against contact, droplet and airborne transmission in patient care.
2. Care
2.1. Assessment
- General condition: consciousness (AVPU scale), skin, mucous membranes, edema, hemorrhage, body temperature, height and weight.
- Respiration: unobstructed airway, breathing (spontaneous breathing, oxygen support, ventilation), respiratory frequency, respiratory pattern, secondary respiratory muscle contractions, cough, noisy breathing and SpO2. If ventilated: ventilator settings.
- Circulation: pulse frequency, pulse volume, pulse, heart anomalies, warm extremities, capillary refill time, blood pressure, central venous or peripheral line, and drugs/ fluids in use.
- Digestion: vomit, nausea, soft abdomen, abdominal distension, eating or enteral tube feeding, daily meal quantity and intake, remaining stomach fluids, defecation.
- Urology: urine color and output, urinary catheter?
- Neurology: muscle contractions, pupils, fontanel.
- Signs: headache, muscle and joint pain.
- There is risk of infection from direct contact with the child, environmental surfaces, medical and care equipment (ventilators, monitors, pulse oximeters, etc.), wastes; droplets from close contact (< 2 meters); and the air when performing aerosol generating procedures on the child (open sputum suctioning, NIV, etc.).
2.2. Care
2.2.1. Respiratory assurance
* For those without respiratory failure
- Place the child in a comfortable position suitable for their age and not obstructing their airway.
- Monitor their general condition, vital signs, fever, cough and respiratory tract infection 2 - 4 times a day and where necessary. To minimize unnecessary contact, healthcare workers may monitor the child via camera or communicate with the child’s caregiver via the bedside speaker or phone.
- Nose and throat hygiene:
+ For older children: instruct them on how to clean the mouth and throat with NaCl 9‰ solution or mouthwash.
+ For young children: clean their nose and mouth using NaCl 9‰ solution.
* For those with respiratory failure
For children receiving oxygen support
- Elevate the child’s head to 30 degrees, let the child lie in a comfortable position and suction sputum where necessary.
- Provide oxygen with suitable flow rate to reach SpO2 ≥ 94% via mask or nasal cannula. When the child’s condition has stabilized, adjust rate to reach SpO2 ≥ 90%.
- Monitor general condition, vital signs and SpO2 every 3 hours and where necessary depending on the child’s condition. Inform the doctor of any anomaly.
- Evaluate the airway, respiratory pattern, oxygen support efficiency and development of the illness.
- Clean the nose and mouth using NaCl 9‰ solution.
For mechanically ventilated children
- Elevate the child’s head to 30º- 45º, use closed sputum suctioning system.
- Evaluate the following every 30 minutes - 1 hour depending on the child’s condition and inform the doctor of any abnormally:
+ Vital signs, SpO2, chest movements, skin color, mucous membranes and consciousness (AVPU scale).
+ Fluid input - output balance
- Change the child’s position every 4 - 6 hours, provide dental care daily.
- Take care of the ventilator and heat and moisture exchanger, ensure that the system is closed and prevent condensation in the circuit. Closely monitor the ventilator’s values.
- Promptly detect and handle ventilator-related accidents.
- Monitor other matters such as ventilator resistance, endotracheal tube obstruction or slipping, pressure ulcers and other anomalies, and report to the doctor.
- Use closed sputum suctioning system (to prevent airborne transmission) and observe sputum quantity, color and properties.
2.2.2. Body temperature control
- Check the child’s temperature on a daily basis and notify the doctor if there is any abnormally. If the child has fever:
+ Loosen the child’s clothes.
+ Place the child in a well-ventilated cool room (air-conditioners are not recommended).
+ Place a warm compress on the forehead, in the armpits and in the groin.
+ Have the child drink a lot of water (ORS, fruit juice, etc.).
+ Administer paracetamol with a dosage of 10 - 15 mg/ kg body weight every 4 - 6 hours when the fever is ≥ 38º5.
2.2.3. Superinfection prevention
- Clean the respiratory tract (use eye and nose droplets), bathe and change clothes on a daily basis.
- Wash hands at the five moments of hand washing when taking care of the child. Ensure all nursing interventions are carried out in a sterile manner.
- Administer oral or injectable antibiotics (if any) according to physician orders.
- Prevent complications related to ventilation, central venous line, venous thrombosis, ulcers, etc. (if any).
2.2.4. Nutrition assurance
- Evaluate the child’s nutritional status to provide a suitable diet.
- Provide the child with liquid, digestible and vitamin-rich food. Food must be fully cooked and contain all necessary nutrients.
- For breastfed children, have the child breastfed both day and night. Provide the mother with nutritional care and supplementary formula.
- If the child cannot eat or has respiratory failure, provide enteral tube nutrition.
- Carry out transfusions according to physician orders (if any).
2.2.5. Health advice and education
- The child’s caregiver may monitor the child’s fever, dry cough, fatigue and muscle pain. If the child develops any of these symptoms, transfer them to an adult healthcare establishment for examination and treatment according to regulations.
- Evaluate psychological development of the child and their caregiver during their stay in the healthcare establishment and give them encouragement as suitable. Explain about the disease and instruct them on how to learn more about the COVID-19 situation via mass media.
- Guidance on infection prevention:
+ Instruct the child on how to wear face masks and replace face masks daily or immediately when the mask gets wet.
+ When the child coughs or sneezes, cover their nose and mouth with a disposable tissue paper and then discard it in the garbage bin according to regulations.
+ Practice hand hygiene regularly using soap or hand sanitizer, avoid letting the child touch their own eyes, nose and mouth.
+ The child’s caregiver shall wear sufficient PPE, including a face mask, headwear, protective clothing and safety goggles or face shield.
+ Avoid hugging or holding the child where unnecessary.
+ Discard waste properly.
2.3. Assessment
Good progress:
- Improved clinical symptoms, stable vital signs, good general condition, normal blood test results and better lung X-rays and at least 2 negative SARS-CoV-2 tests.
- The child and their family understand about COVID-19, care methods and how to prevent the disease.
- Healthcare workers and the child’s caregiver are not infected with the disease.
No progress or worsening:
- The child’s general condition makes no progress or worsens. The child develops respiratory failure signs or worsened respiratory failure, functional disorders, complications such as superinfection, pressure ulcers, etc. or spreads COVID-19 to healthcare workers and their caregiver.
APPENDIX
OXYGEN THERAPY PROCEDURES
|
No. |
Step |
Requirement and purpose |
|
A. Nasal cannula/ Nasopharyngeal cannula oxygen |
||
|
1 |
Nurse wears PPE. |
N95 mask fits properly to the face. |
|
2 |
Prepare all necessary equipment |
|
|
3 |
Evaluate the patient’s condition, pay attention to the patient’s respiratory and circulatory conditions. Explain the procedure’s purpose to the patient (if possible). Place the patient in a suitable position. Loosen the patient’s clothes and suction sputum (if necessary). |
Identify the correct patient. |
|
4 |
Unlock, check oxygen equipment, clock and humidifier. |
|
|
5
|
Disinfect hands; connect the nasal cannula with oxygen system. |
|
|
6 |
Adjust oxygen flow rate as indicated. Check oxygen flow on dorsum of the hand or in a glass of water. |
Check if oxygen flow rate is set as indicated by doctor. |
|
7 |
Place nasal cannula on the patient’s nasal bridge (cannula tab facing downwards). Insert a nelaton catheter through the nose into the nasopharynx. |
Perform the tasks gently. |
|
8 |
Secure lower part of the cannula to the patient’s head or chin/ secure nelaton catheter to the nostril or cheek. |
Change location where the cannula/ catheter is secured. |
|
9 |
Check and adjust oxygen flow rate as indicated by doctor. |
Follow doctor’s indication. |
|
10 |
Monitor the patient’s condition and oxygen system. |
Prevent the cannula/ catheter from folding, being obstructed or dislocating. |
|
11 |
Recollect equipment: Sort biomedical wastes. Move dirty equipment to the cleaning room and handle according to regulations. |
Wastes and equipment must be disinfected before being moved to storage. |
|
12 |
Return other equipment to its location (after disinfection) |
Ensure they are available for emergency use. |
|
13 |
Remove PPE in the anteroom and wash hands |
Seriously take measures to prevent transmission. |
|
14 |
Update the care sheet (if the patient’s medical record is available electronically, immediately update the record in the patient’s room and print it outside of the room; otherwise, communicate via handheld transceivers with workers outside of the patient’s room to update the medical record). |
Reduce transmission to healthcare workers inside the healthcare establishment. |
AEROSOL DRUG DELIVERY PROCEDURE
|
No. |
Step |
Requirement and purpose |
|
1 |
Healthcare workers wear PPE. |
Wear N95 masks; wear face shields. |
|
2 |
Check operation of aerosol generating equipment. Prepare equipment |
Prepare and check all equipment before entering the patient’s room. |
|
3 |
Identify the correct patient. Evaluate respiratory condition, vesicular breathing, lung rales. Pulse, blood pressure Explain the procedure to the patient. Place the patient in a suitable position. |
Patient sits comfortably/ patient’s head is elevated (600-900). |
|
4 |
Nurse wears a second pair of gloves and fills a syringe with the drug according to physician order. |
Check “5 right’s”. |
|
5 |
Use the syringe to dispense the dose to a cup containing NaCl 0,9%. |
According to doctor’s indication. |
|
6 |
Connect the aerosol mask or jet nebulizer to the drug cup. |
|
|
7 |
Place the mask onto the patient’s face and adjust the strap to fit the mask to the nose and mouth or place the jet nebulizer to the patient's mouth. |
Ensure that the mask fits the nose and mouth properly/ the jet nebulizer is properly placed in the patient’s mouth. |
|
8 |
Turn the aerosol generating equipment on. Instruct the patient on how to perform the procedure properly. |
Exhale with maximum effort. Inhale slowly and deeply. Exhale slowly. Repeat until the drug in the cup is finished. |
|
9 |
Disconnect the aerosol mask or jet nebulizer and the drug cup from the aerosol generating equipment. Disinfect the aerosol mask or jet nebulizer and drug cup. Disinfect surfaces of the aerosol generating equipment. |
Disinfect before moving the equipment from the patient's room to the disinfection area. |
|
10 |
Evaluate the patient’s condition after using aerosols. |
|
|
11 |
Wastes |
Disinfect and label wastes as COVID-19 dangers before moving them to waste storage area. |
|
12 |
Remove PPE in the anteroom and wash hands. |
|
|
13 |
Update the care sheet (if the patient’s medical record is available electronically, immediately update the record in the patient’s room and print it outside of the room; otherwise, communicate via handheld transceivers with workers outside of the patient’s room to update the medical record). |
Reduce transmission to healthcare workers. Include initial data such as time, patient’s condition and patient evaluation after aerosol use. |
SPUTUM SUCTIONING PROCEDURE
PROCEDURE:
|
No. |
Step |
Requirement and purpose |
|
A. Upper respiratory tract suctioning (mouth - nose) |
||
|
1 |
Wear PPE. |
Cover the whole body. |
|
2 |
Prepare equipment (On trolley or shelf secured at bed head). |
Ensure that all equipment is available before performing the procedure/ entering the patient’s room. |
|
3 |
Explain the procedure’s purpose to the patient. Evaluate patient’s condition. Place the patient’s head on its side (if possible). |
Identify the correct patient. Prevent choking as it may stimulate vomiting. |
|
4 |
Nurse wears clean gloves. |
|
|
5 |
Connect the suction catheter with the suction machine. Turn the machine on and check suctioning pressure. |
Infants: from -60 to -80 Children: from -80 to -100 Adults: from -80 to -120 (unit: mmHg) |
|
6 |
Perform suctioning: Oral suctioning: insert the suction catheter 4-6 cm into the inside corner of the jaw and into the Mayo tube. Nasal suctioning: insert the suction catheter into both nostrils and move it along the septum and palate until it reaches the nasopharynx (approximately 7-8 cm). Start suctioning by pushing down on the valve. Suction intermittently and twist the catheter while withdrawing it gently. |
Insert gently; do not suction. When inserting the catheter, do not move it up or down to avoid injuring the mucous membrane. Monitor the patient’s facial expression, SpO2, pulse, etc. while suctioning. |
|
7 |
Clean the catheter and repeat suctioning until all sputum has been removed. |
|
|
8 |
Turn the suction machine off; remove the suction catheter and soak it in a bucket containing disinfectant solution. |
Prevent hospital-acquired infection. |
|
9 |
Place the patient in a comfortable position. |
|
|
10 |
Replace the bottle containing catheter cleaning solution. |
|
|
11 |
Recollect equipment: Sort biomedical wastes. Move dirty equipment to cleaning room and handle according to regulations. Return other equipment to its location. Clean and disinfect surfaces. |
Disinfect, place in tightly closed containers, label as COVID-19 dangers and move to disinfection area. |
|
12 |
Update the care sheet (if the patient’s medical record is available electronically, immediately update the record in the patient’s room and print it outside of the room; otherwise, communicate via handheld transceivers with workers outside of the patient’s room to update the medical record). |
Reduce transmission to healthcare workers. |
|
B. Lower respiratory tract sputum suctioning via endotracheal or tracheostomy tube |
||
|
1 |
Wear PPE. |
|
|
2 |
Prepare all necessary equipment. (On trolley or shelf secured at bed head). |
Check all equipment before entering the patient’s room. |
|
3 |
Explain the procedure’s purpose to the patient (if possible). Clap and vibrate from lower lobes in 3 positions (if possible). Evaluate FiO2, SPO2, PEEP (for mechanically ventilated patients); diagnose tetanus and increased intracranial pressure. Check cuff pressure. Increase FiO2 to 100% before, during and after 3 minutes of suctioning (for mechanically ventilated patients). |
Help loosen sputum for effective suctioning. Prevent endotracheal or tracheostomy tube from slipping. Prevent oxygen loss during suctioning. Ensure SpO2 > 90%. |
|
3 |
Explain the procedure’s purpose to the patient (if possible). Clap and vibrate from lower lobes in 3 positions (if possible) or in prone position (for special cases). Evaluate FiO2, SPO2, PEEP (for mechanically ventilated patients); diagnose tetanus and increased intracranial pressure. Check cuff pressure. Increase FiO2 to 100% before, during and after 3 minutes of suctioning (for mechanically ventilated patients). |
Help loosen sputum for effective suctioning. Prevent endotracheal or tracheostomy tube from slipping. Prevent oxygen loss during suctioning. Ensure SpO2 > 90%. |
|
4 |
Open suction catheter in advance (for open suction catheter). Nurse wears sterile gloves or clean gloves for closed suction catheter. Connect the suction catheter with the suction machine. Turn the machine on and check suctioning pressure. |
Infants: from -60 to -80 Children: from 80 to -100 Adults: from 80 to -120 (unit: mmHg) |
|
5 |
Perform suctioning: Insert the suction catheter gently until it touches the mucous membrane to stimulate coughing. Withdraw the catheter by 1-2cm and start suctioning (by pushing down on valve). Twist the catheter while withdrawing it gently. Suction in 3 positions (if possible). |
Ensure sterilization. Comply with “clean hand” rule: after wearing sterile gloves, the hand holding the suction catheter shall only hold the catheter without touching anything else. Do not suction while inserting the catheter. During suctioning, do not move the catheter up or down to avoid injuring the mucous membrane. Monitor the patient’s facial expression, SpO2, pulse, etc.. Each suctioning shall last for 10-15 seconds. Do not suction continuously. Reconnect the patient to the ventilator to achieve SpO2 > 90%. Upon end of suctioning, ensure SpO2 is stable and adjust FiO2 to starting value. |
|
6 |
Repeat suctioning until all sputum has been removed. |
|
|
7 |
Turn the suction machine off; remove the suction catheter and soak it in a bucket containing disinfectant solution. |
Prevent hospital-acquired infection and cross-contamination. |
|
8 |
Place the patient in a comfortable position. |
|
|
9 |
Replace the bottle containing catheter cleaning solution. |
|
|
10 |
Recollect equipment: Sort biomedical wastes. Move dirty equipment to cleaning room and handle according to regulations. Return other equipment to its location. Disinfect surfaces. |
Disinfect, place in tightly closed containers, label as COVID-19 dangers and move to disinfection area. |
|
11 |
Remove PPE in the anteroom and wash hands. |
|
|
12 |
Update the care sheet (if the patient’s medical record is available electronically, immediately update the record in the patient’s room and print it outside of the room; otherwise, communicate via handheld transceivers with workers outside of the patient’s room to update the medical record). |
Reduce transmission to healthcare workers. |
DENTAL CARE PROCEDURE
|
No. |
Step |
Requirement and purpose |
|
1 |
Wear PPE. |
Cover the whole body; wear face shields. |
|
2 |
Prepare all necessary equipment. |
Check all equipment before entering the patient’s room. |
|
3 |
Explain the procedure’s purpose to the patient and their family (if possible). Place the patient on their side. |
|
|
4 |
Wrap a towel around the patient’s neck and place a kidney tray next to the patient’s cheek. |
Do not wet the sheets or patient’s clothes. |
|
5 |
Nurse disinfects hands. |
|
|
6 |
Open care kit. Pour solutions into stainless steel bowls: 01 bowl of saline, 01 bowl of mouthwash such as chlorhexidine 0,12%, povidone, Listerine, Givalex, etc. Put gauze sponges in care kit. |
|
|
7 |
Nurse wears clean gloves. |
|
|
8 |
Remove dentures (if any). Perform physical examination and evaluate patient's condition. |
Evaluate consciousness. Check cuff pressure. Endotracheal or tracheostomy tube. Examine patient’s mouth according to BRUSHED. |
|
9 |
Start providing dental care: Use tweezers to dip gauze sponges in NaCl 0,9% solution, use a pincer to wash the patient’s teeth from the upper set, lower set, lingual side, incisal side, occlusal side, tongue, palate, inside sides of the jaws to the gum. Use a tongue depressor to open the patient’s mouth for easy access. Replace gauze sponges and clean multiple times. Soak round sponges in chlohexidine 0,12% solution and wipe the teeth, tongue and gum. |
Ensure sterilization in case of oral injury. For comatose patients, be careful when soaking gauze sponges to prevent choking. Use a syringe to clean the mouths of patients who cannot spit or gargle and suction the liquid afterwards. Do not wash the mouth after using disinfectant. |
|
9 |
Dry the mouth and clean the face. |
Clean both eyes first. |
|
10 |
Apply Glycerine/Vaseline to patient’s lips to alleviate dryness. |
After cleaning. |
|
11 |
Place the patient in a comfortable position. |
|
|
12 |
Recollect equipment: Sort biomedical wastes. Move dirty equipment to cleaning room and handle according to regulations. Return other equipment to its location. Disinfect surfaces. |
Disinfect, place in tightly closed containers, label as COVID-19 dangers and move to disinfection area. |
|
|
Remove PPE in the anteroom. |
|
|
|
Update the care sheet (if the patient’s medical record is available electronically, immediately update the record in the patient’s room and print it outside of the room; otherwise, communicate via handheld transceivers with workers outside of the patient’s room to update the medical record). |
Reduce transmission to healthcare workers. |
TABLE OF CONTENTS
Overview on SARS-CoV-2
Management of COVID-19 cases
Prevention of infection in care of COVID-19 cases
Care of suspected, asymptomatic, mild and moderate COVID-19 cases
Care of severe and critical COVID-19 cases
Care and management of pregnant women suspected or confirmed to have COVID-19
Care of children suspected or confirmed to have COVID-19
Appendix